Home » Posts tagged 'exercise'
Tag Archives: exercise
Is Diet and Exercise Eugenic?
1550 words
Eugenics can be defined as “the science of improving a human population by controlled breeding to increase the occurrence of desirable heritable characteristics.” Though, in his book Genetic Ethics: An Introduction, Farrelly (2018: 30) cites Bertrand Russel’s definition of eugenics. Eugenics is “the attempt to improve the biological character of a breed by deliberate methods adopted to that end.” So, eugenics does not have to be ‘bad’, if it is morally justifiable and defensible, if they treat all people as free and equal (which most eugenic movements in the past have not done. See my article Eugenics and the State for a history of eugenics and the policies that arose from it.)
Dieting (defined as “what one eats”, not the other commonly-used definition “when one is in caloric restriction under TDEE”) and exercise change the expression of genes in the genome. For example, mature skeletal muscle can adapt to numerous stressors—indeed, if it could not, then we would not be able to choose to gain (or lose) muscle mass. Exercise induces the activity of certain genes (Vissing, Anderson, and Schjerling, 2005). One study on endurance athletes showed that there are pronounced effects of gene expression on exercised and non-exercised muscles (Catoire et al, 2012). One study showed that the ingestion of glucose during exercise decreases the gene expression of genes associated with fatty acid metabolism (Civitarese et al, 2005). Numerous epigenetic changes are also induced by exercise (Ntanasis-Stathopoulos, Tzanninis, and Koutsilieris, 2013). Miyamoto-Mikami et al (2018) showed that young men who participated in high-intensity intermittent exercise training showed that 79 genes had an elevated expression whereas 73 genes were significantly reduced.
Williams and Neufer (1996) show that long-term responses in regard to adaptations in regard to a specific exercise “require changes in gene expression, mediated by changes in the rate of transcription of specific genes and in the rate of synthesis of
specific proteins.” Further, diet and exercise can change the transcriptional properties of skeletal muscle, which induce further physiological changes (Hargreaves and Cameron-Smith, 2002). There is even preliminary evidence that diet and exercise affects the epigenome over several generations (Barres and Zierath, 2016). Since changes occur to the epigenome due to environmental stressors, and exercise is an environmental stressor, it follows that exercise, too, can change the epigenome.
People visit the gym to change their biology. Since people visit the gym to change their biology, are they involved in “self-eugenics”? I would say yes, going with the definition from Russell quoted above. That one wants to change their biology means that they are most likely not currently happy with the way their biological phenotype currently is. So they visit the gym, begin a diet (defined here as “caloric restriction”) in order to change their biological phenotype since they are not happy with it. Methods like diet and exercise seek to improve the biological character of a breed through deliberate methods, and so, fall under the umbrella of “eugenics.”
But there is a difference between this type of “eugenics” and methods commonly thought of when “eugenics” are discussed. “When eugenic measures exemplify moral and epistemic virtue rather than vice, they are morally obligatory rather than simply morally permissible” (Farrelly, 2018: 42). Prescribing (a sensible) diet and exercise to a populace can and will improve their health; further, educating people on the right and wrong things to eat (“right and wrong things to eat” in regard to their current goals) and how these things we eat affect our physiology is not morally objectionable nor is it coercive.
Think of the eugenic policies I discussed in my article on eugenics and the State. The policies discussed (such as forced sterilization, infanticide, forced contraceptive measures, and selective breeding) are immoral: the State is attempting to force its ideals on the populace, and so it can be argued that it is immoral since individual autonomy is taken away (or attempted to be taken away). On the other hand, prescribing diet and exercise is not eugenic in this manner: it’s just a prescription, what one should do if they would like to live their life to the highest quality. This includes staying away from highly processed and refined foods (carbs) and other, “non-natural” foodstuffs. This is only a suggestion based on the current state of nutritional knowledge; if one wants to live the best-possible life then they should diet and exercise.
On the other hand, we can take a State-measure and, using the definition in this article from Russell, can say that this measure is eugenic, but its similarities to what is being argued here is irrelevant, since I am arguing for education, not forcing people to do something (though I will state my views on this matter at the end, which I still honestly think about since it conflicts with some of my views.)
Back in the beginning of this decade, then-mayor of NYC Michael Bloomberg “proposed [a] regulation that would bar food service establishments from selling certain sugary drinks in containers larger than sixteen ounces” in an effort to “reduce the city’s obesity rate.” When this law was proposed, I was all for it. People cannot make decisions for themselves, because when they do, they make the “wrong” (in regard to, what I would assume to be what people try to achieve—a healthy lifestyle) decisions, and so, I thought that a policy like this was a good idea, because who the hell needs a 64 oz. Big Gulp soda (which could have up to 700 kcal in the cup) from 7-11? Why would someone need to down almost 2 liters of soda in one go? Note that, I would assume, the individual would not be caught dead drinking out of a 2-liter bottle of soda (though I have seen quite a lot of people do so, even early in the morning). But there is no problem using the cup since its size is kind of deceptive—deceptive in the manner that it does not look like the 2-liter bottle of (family-sized) soda.
I loved this proposal when it was announced. It would, I thought, attempt to address one aspect of our obesity problem (since nearly 40 percent of all of the added sugars we consume come from sugary drinks). Back then, I was more libertarian in my politics, but I thought that the policy was a good idea, even though it conflicted with my views on politics. I now do not believe we should take these types of measures—I believe that education is sufficient, along with getting rid of food deserts which hamper the ability of those in those deserts to get access to good, high-quality food (which affects certain races over others; National Research Council, 2009).
The view held by Bloomberg, and now current NYC mayor Bill Deblasio, is an example of a policy that would take away one’s choice to drink what they would like. Bloomberg’s rationale was that, if people wanted more of the drink, then they can go over and refill their cup so that they can see what and how much they are actually drinking. This, on its face, is sensible. If one wants to drink the same amount they would have drank in, say, a 64 oz. Big Gulp, they can keep refilling their cup in order to get the same amount of liquid they would have gotten in the bigger cup. But, what if someone wants a 64 oz. Big Gulp? What about a 128 oz. Ultra Big Gulp? A 256 oz. Super Ultra Big Gulp? Is there anywhere we should draw this line? Should we?
In any case, I have shown that exercise and diet is “eugenic” in the sense of Russel’s definition. But it is not “eugenic” in the sense of, in my opinion, what most people mean when they discuss “eugenics”: taking away one’s individual autonomy to do what they want, forcing them to do something. (Though, they are not being told they cannot drink sugary drinks, they are being told that there is a size limit on how big their cup is; they would be forced to drink a sugary drink in a small cup.)
Bloomberg’s proposed measure is quite obviously eugenic since it “attempt[s] to improve the biological character of a breed by deliberate methods adopted to that end.” Is the health of the populace more important than individual autonomy to be able to buy their 256 oz. Super Ultra Big Gulp? Or is one’s ability to freely drink their 256 oz. Ultra Big Gulp more important? If it can be shown that this policy would reduce the number of obese people in the City, should it be attempted?
These are important (moral) questions to answer. I am honestly undecided here; this issue is incredibly complex. Though, we do know one thing: exercise and diet is “eugenic” in Russel’s sense, and the measures exemplify moral and epistemic virtue so it is not like “State-forced” eugenics of old. Whether or not there is a negative connotation to “eugenics” depends on whether or not it pursues sound and morally justifiable aims. Therefore, though prescribing diet and exercise is eugenic since they both influence the epigenome and gene expression (along with it falling under Russel’s definition of eugenics), it is not eugenic in a negative sense, since there are sound and morally justifiable aims in prescribing diet and exercise to the population at large.
Strength and Neuromuscular Coordination
2250 words
PumpkinPerson (PP) has some weird—and uneducated—views regarding strength and coordination, which, of course, implies that he has no understanding of what “coordination” truly is. He seems to have convinced himself that coordination weightlifting does not require coordination (neuromuscular coordination; hereafter NMC—the ability of the central nervous system—CNS—to control muscles). That view is patently ridiculous. In this article, I will explain the logic behind the fact that strength and power exercises, in particular, NEED a high NMC, and without a high NMC, the athlete in question cannot perform to their highest potential.
PP wrote about an “athletic g factor” to attempt to liken it to the “g factor” regarding “intelligence” tests, but I’m not worried about that comparison (IQ is boring to me now). What I am worried about are his outlandish claims regarding what he believes regarding strength and NMC. PP cited Jensen’s Bias in Mental Testing where Jensen cited a correlation matrix in which “all of [the] correlations were positive“, writing that he’s “not sure why some commenters think weight lifting requires coordination when the correlation between strength (hand grip, chinning) and coordination (Pursuit rotor tacking, Mirror star tracing) is zero” (PP; Physical Coordination).
Well, “some commenters” have actual experience in what he is talking about, so, forgive me if I don’t believe the claims that, in my opinion, he pulled out of thin air. Take chin-ups. Imagine a case of someone attempting to chin-up that does not have high NMC. Since they were not coordinated, do you think they would be able to do a controlled rep in order to complete one rep? Or would their body be all over the place, flailing around since they do not have the mind-muscle (MMC) connection required to complete the lift. Now take his other example, hand grip. On its face, one might assume that this requires no NMC. But think about the process of gripping something tightly. If the muscles in the forearm, for example, are not adequately trained, then, in all lifts involving forearm strength (a great majority of which involve at least some type of forearm strength) will not be able to be performed properly, since the individual in question does not have the NMC required to properly do the exercise in question.
PP then says that when he “lift weights, [he doesn’t] feel like [he’s] using coordination.” This proves two things to me: (1) PP does not know how to lift properly, and then (2) follows that he does not know about the MMC.
The MMC is where the mind and the body “meet.” Acetylcholine functions as a neurotransmitter. This neurotransmitter “communicates” with the muscles in the body to cause a contraction. This contraction, then, causes the action of voluntary muscle movement. (I had an A&P professor explain to me that, out of the whole textbook he taught out of, one of the only things in the textbook that we could choose to do was move the body—contract muscles and cause movement). So when acetylcholine is released, it latches onto muscle fibers and causes muscle contractions.
We can put the MMC in this way: imagine doing a movement such as a bicep curl. One is not actively attempting to use the proper levers in order to properly lift the weight. On the other hand, if one is actively thinking about the muscles being used in the movement, then they are using the connection—they are strengthing their MMC and, in turn, developing the proper NMC which is required in order to properly lift weights and get the most returns possible from your time spent lifting.
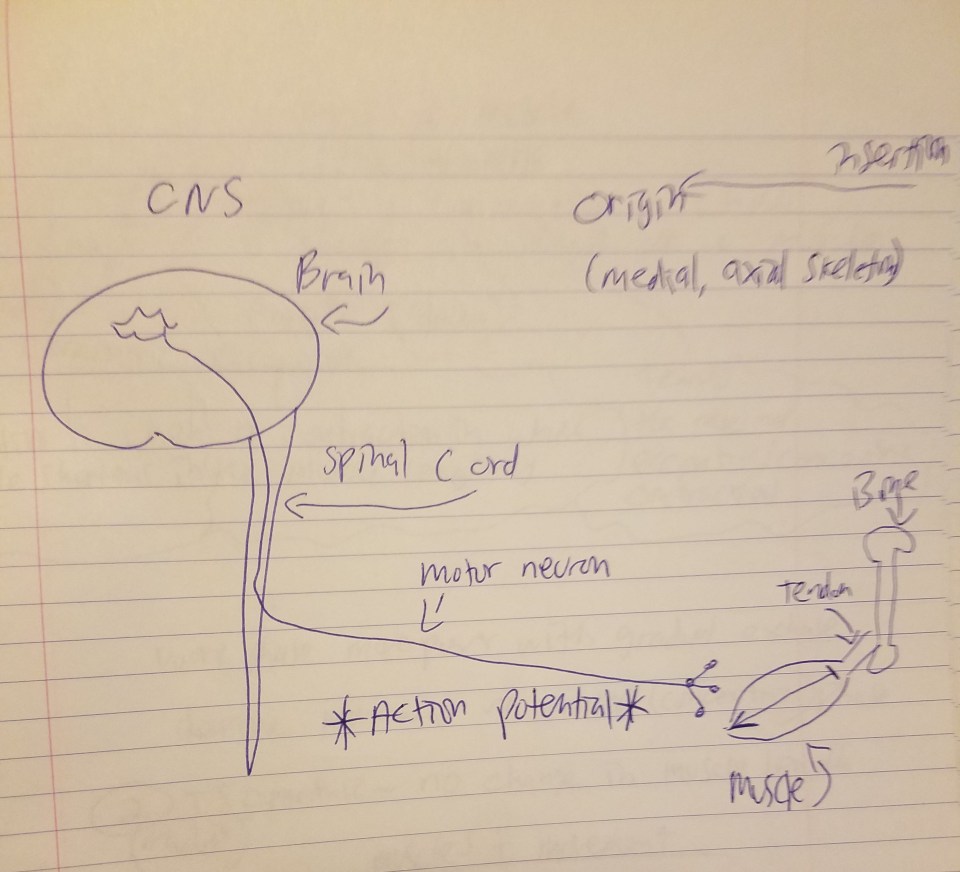
The above diagram I drew is the process by which muscle action occurs. In my recent article on fiber typing and metabolic disease, I explained the process by which muscles contract:
But the skeletal muscle will not contract unless the skeletal muscles are stimulated. The nervous system and the muscular system communicate, which is called neural activiation—defined as the contraction of muscle generated by neural stimulation. We have what are called “motor neurons”—neurons located in the CNS (central nervous system) which can send impulses to muscles to move them. This is done through a special synapse called the neuromuscular junction. A motor neuron that connects with muscle fibers is called a motor unit and the point where the muscle fiber and motor unit meet is callled the neuromuscular junction. It is a small gap between the nerve and muscle fiber called a synapse. Action potentials (electrical impulses) are sent down the axon of the motor neuron from the CNS and when the action potential reaches the end of the axon, hormones called neurotransmitters are then released. Neurotransmitters transport the electrical signal from the nerve to the muscle.
So action potentials (APs) are carried out at the junction between synapses. So, regarding acetylcholine, when it is released, it binds to the synapses (a small space which separates the muscle from the nerve) and it then binds onto the receptors of the muscle fibers. Now we know that, in order for a muscle to contract, the brain sends the chemical message (acetylcholine) across synapses which then initiates movement. So, as can be seen from the diagram above, the MMC refers to the chemo-electric connection between the motor cortex, the cortico-spinal column, peripheral nerves and the neuromuscular junction. A neuromuscular junction is a synapse formed by the contact between a motor neuron and a muscle fiber. This is why beginners in the gym get stronger in the first 8 weeks or so of training—there has not been enough time for muscle to adequately grow in that time span. Thus, when people lift weights correctly, what they are doing is training their NMC—and their mind—to be able to adequately perform these types of actions in a safe, controlled manner.
How is NMC measured? It’s not simple to measure it, and in reality, the most feasible way to “measure it” in real life situations without the use of a lab is to just see one’s progress while they progress through higher and higher weights from their starting weights and they learn to perform the exercise in question safely. But a more empirical measure used in order to measure NMC are electromyography (EMG) tests. In fact, this test is THE MEASURE used to measure NMC, since all of the relevant variables in question (some seen in the above diagram) are tested. EMGs are used for numerous reasons, mostly in order to test for types of motor diseases which affect muscle action. There is also a related measure here: a nerve conduction study. This measures the speed and strength of signals traveling between two synapses, and so, the better one’s nerve conduction is in regard to muscle action, the higher their NMC is and, therefore, the better they will be able to perform any certain lift. So, for example, we can say that one’s NMC increased and the cause was resistance training if their EMG tests increase.
Imagine an Olympic lifter going to snatch 400 pounds. Would any sane person bet that they have low NMC (i.e., a low rate of firing between synapses as measured by an EMG)? A claim such as this would be quite preposterous—individuals like Olympic lifters clearly have trained both their bodies and minds in order to lift to the best of their abilities. And if they did NOT have high NMC (i.e., a higher rate of firing between synapses), then the weight would wobble and ultimately fall, causing the lifter serious injury. But, of course, we do not see that, since strength and NMC are closely related.
I now have some examples of studies which looked into this matter (that thinking about the action one is performing activates the primary muscles used in the movement in question), which will definitely put PP’s claims to rest for good.
Neuromuscular coordination is needed, for example, to be able to “squat lift” correctly (meaning, pick up a load from a squatting start and lift it; Scholz, Millford, and McMillan, 1995). Our understanding of how this occurs has greatly increased in 30 some-odd years since our technology has improved.
Now, take the MMC. We can simply define it as “One focusing on using the muscles in question to perform the lift.” Calatayud et al (2016) studied 18 resistance-trained men on a 1RM (one-rep max) bench press. Each individual in the study participated in 2 sessions: one to determine their 1RM and another experimental session. Calatayud et al (2016) attempted to control for as many factors as possible in order to attempt to see if the baseline changed at all. For example, all measures were made by the same two investigators; all measures were taken in the same facility; all participants participated in the same warm-up mobility drills prior to performing the lift; all participants performed the lift in the exact same manner they performed the two aforementioned sessions (same technique and body position, i.e., suicide grip and powerlifting technique).
They found that (1) higher levels of EMG activity lead to moving more weight; (2) the men could “selectively activate pectoralis and triceps muscles during the
bench press when this exercise is performed at low intensities” (Calatayud et al, 2016), at moderate intensities; (3) that focusing on one muscle (i.e., triceps brachii over pec major) did not hamper activation in one over the other; and (4) a threshold exists between 60-80 percent existed for muscle activation. Thus, experienced resistance-trained men can actively increase activity in certain muscles when cued to focus on those certain muscles.
Snyder and Fry (2012) studied 11 D-III football players on the bench press while recording EMG activity. They found that, when verbal cues were given to focus on the chest muscles, EMG increased by 22 percent, but when verbally cued to focus on the triceps, the pec major returned to baseline (though this does not mean, of course, that performance was hampered), while EMG activity increased by 26 percent. However, in-line with the findings from Calatayud et al (2016), when 80% 1RM were tested, EMG activity in the triceps remained unchanged, implying that there is a threshold.
The results of this study show that trained subjects can alter the participation of muscles in both moderate and higher-intensity multijoint resistance training exercises in response to verbal instructions, because both TB and PM activities were increased selectively in response to 2 different sets of instructions at 50% 1RM and 80% 1RM. This indicates that verbal instructions from trainers, therapists, and coaches are likely to have a measurable effect on muscle involvement, although it is unclear how generalizable this effect might be to all training exercises. Previous research from our laboratory (23) indicated that untrained subjects performing a lat pull-down at 30% max isometric load could respond to verbal instructions to increase back muscle involvement by increasing latissimus dorsi activity while maintaining proper form and similar speed of movement. The subjects in that study increased latissimus dorsi activity by 17.6%, whereas in the current study, verbal instruction resulted in a 22.3% increase from baseline at 50% 1RM for PM and a 25.6% increase for TB. However, antagonist activity was not measured by Snyder and Leech (23), and it was possible that the subjects activated antagonist muscles to offset additional force produced by agonist muscles. This study addressed this possibility, but no changes were seen in antagonist muscle activity with verbal instructions. The question of the effect of higher testing loads was also addressed by this study, and it was found that at 50% 1RM, the subjects were capable of altering muscle participation of both the horizontal adductors and the elbow extensors, but at 80% 1RM, only the horizontal adductors were affected. (Snyder and Fry, 2012)
If the activity of a muscle as measured by EMG is increased, then we can say that, for all intents and purposed, that NMC is high. One who is not familiar with a lift will have low NMC, that is, the firing will be low compared to someone with high NMC. Quite clearly, verbal instruction to focus on certain muscles can better activate them, and, using EMG, we can say that they have high NMC if the firing between synapses is fast.
Rutherford and Jones (1986) write that “It is concluded that a large part of the improvement in the ability to lift weights was due to an increased ability to coordinate other muscle groups involved in the movement such as those used to stabilise the body.” How weird is that… While Kim, Lockhart, and Roberto (2009) in their sample of elderly individuals found that “Strength gain by exercise training plays a role in the improved coordination of other fixator muscles necessary for body support while performing daily tasks such as cooking, gardening, reaching for an object, and walking, and in gaining more coordinated contractions between agonist and antagonist muscle groups leading to greater net force in the imposing movements.” Finally, Dahab and McCambridge (2009) found that strength training in kids improves the number and coordination of active neurons along with the firing rate pattern. This is important because the number and coordination of active neurons along with the rate of firing pattern influences—very strongly—NMC and how coordinated they will be.
In conclusion, it is quite obvious that PP does not know what he is talking about and only writes what sounds good in his head without having an adequate understanding of anatomy and physiology, NMC, MMC, APs and the like. These types of confusions can be cleared up by having an adequate understanding of anatomy and physiology and knowing how and why muscle actions are done, where they begin and where they end. Clearly, the claim that weight lifting requires no coordination is false.
On Individual Variation in Response to Exercise
1500 words
On Twitter, JayMan wrote: “Not talked about much by fitness buffs (a world that’s full of BS anyway): a fair fraction of people respond little to even *negatively* to exercise“. This is the same person that thinks behavior genetics is a science, and that is a field “that’s full of BS anyway”, too. Anyway, the article that JayMan cited was from the website Stronger by Science, titled Hardgainers? What We Know About Non-Responders by Greg Nuckols.
First off, JayMan’s comment that “a fair fraction of people respond … *negatively* to exercise” is, on its face, already false. Most everyone in the study referenced by Nuckols (There Are No Nonresponders to Resistance-Type Training in Older Men and Women; Churchward-Venne et al, 2015) gained strength, but some people’s muscle fibers did not grow, and some apparently shrank (that is, their muscle cross-section area; CSA). But the important thing to note is that ALL gained strength, which implies physiologic adaptation to the stressor placed on the body (something that is overlooked).
Though, even if some people do not respond to certain programs or weight/rep schemes, does not mean that they are “non-responders”. All that needs to be done is to change the program if one “does not respond” to the program created. All exercise programs should be tailored to the individual and their own specific goals. There is no “one-size-fits-all” exercise program, as can be seen from these studies on so-called “hardgainers.”
The best study for this matter, though, is the HERITAGE (HEalth, RIsk factors, exercise, Training, And GEnetics) study, carried out by five universities in Canada and the US, who enlisted 98 two-generation families and then subject each member to five months of the same stationary bike training regimen—three workouts per week with increasing intensity. Each of the 482 individuals in the study was assayed, and so we would also see which genes would play a role in how fit one person would be in comparison to another.
David Epstein, author of The Sports Gene, writes (pg 85):
Despite the fact that every member of the study was on an identical exercise program, all four sites saw a vast and similar spectrum of aerobic capacity improvement, from about 15 percent of participants who showed little or no gain whatsoever after five months of training all the way up to 15 percent of participants who improved dramatically, increasing the amount of oxygen their bodies could use by 50 percent or more.
Amazingly, the amount of improvement that any one person experienced had nothing to do with how good they were to start. In some cases, the poor got relatively poorer (people who started with a low aerobic capacity and improved little); in others, the oxygen rich got richer (people who started with high aerobic capacity and improved rapidly); with all manner of variation in between—exercisers with a high baseline aerobic capacity and little improvement and others with meager starting aerobic capaacity whose bodies transformed drastically.
Though, contrary to JayMan’s claims, “Fortunately, every single HERITAGE subject experienced health benefits from exercise. Even those who did not improve at all in aerobic capacity improved in some other health parameter, like blood pressure, cholesterol, or insulin sensitivity” (Epstein, 2014: 88).
Epstein also writes about another study, undertaken at the University of Alabama-Birmingham’s Core Muscle and Research Laboratory, writing:
Sixty-six people of varying ages were put on a four-month strength training plan—squats, leg press, and leg lifts—all matched for effort level as a percentage of the meximinum they could lift. (A typical set was eleven reps at 75 percent of the maxmimum that could be lifted for a single rep.) At the end of the trainin, the sibjects fell rather neatly into three groups: those whose thigh muscle fibers grew 50 percent in size; those whose fibers grew 25 percent; and those who had no increased in muscle size at all.
[…]
Seventeen weight lifters were “extreme responders” who added muscle furiously; thirty-two were moderate responders, who had decent gains; and seventeen were nonresponders, whose muscle fibers did not grow.* (pg 110)
* “It’s important to keep in mind that the harder the training, the less likely there are to be “nonresponders.” The harder the work, the more likely a subject will get at least some response, even if it is less than her peers” (pg 376).
Those who responded the most to the regimen had the most satellite cells in their quads which were waiting to be activated by training. When one becomes stronger from hypertrophy, the muscle thickness correlates to muscle CSA (Franchi et al, 2018). When one performs a repetition, the muscle fibers break down—this leads to trauma of the cellular proteins in the muscles which must then go under repair. Numerous growth factors influence the growth of skeletal muscle, such as GH (growth hormone), testosterone, protein and carb intake. Skeletal muscle adapts almost immediately after a bout of exercise, but the apparent changes to the muscle (both in the mirror and seeing large gains in strength on any particular movement) will take weeks and months.
There’s one thing about the claims of “exercise nonresponders” that really gets me: everyone responds positively to exercise, even if it’s not the same exact response to another individual doing the same—or different—exercise! I don’t know who made the claim that “people respond the same to any exercise program”, but that’s a claim that hbdchick made, writing “plenty of the “fitness buffs” do [make the claim that everyone would respond the same to the same exercise regimen]. I then asked her, and JayMan, to name three people who made this outrageous claim: but, of course, I got no answer.
Not to mention that Nuckols ended the article writing:
… there were way fewer nonresponders when people were put on personalized training programs instead of one-size-fits-all standardized programs. This study was primarily looking at aerobic fitness, but it also examined strength measures (bench press and leg press 5RM). It found that all the subjects on personalized programs got stronger, while only 64.3% of the subjects on standardized programs got stronger. This gives us more evidence that “nonresponders” in scientific studies aren’t necessarily “true” nonresponders.
Take two people who have similar measures and, say, start at the same weight on one exercise. In 6 months, all else being equal with regard to lifestyle, there will be a difference in strength gained on that particular exercise. However, an increase from t he baseline from when both individuals began, to the 6-month point, shows that they did, indeed, respond to the exercise program at least in some way (see above quotes from Epstein). Thus, the claim that “there are nonresponders to exercise” makes no sense, on the basis that people necessarily respond physiologically to the stressors placed on them, and so, if they do more (and they will) than they did previously from their baseline, then they did adapt to the protocol, implying that they are not “nonresponders” to exercise. It does not matter if Person B does not catch up to Person A on all variables: the fact that there was a difference in each individual from the baseline all the way to 6 months on a specific regimen implies adaptation to the stressors—which implies that there is no such thing “nonresponders”.
JayMan also has views similar to this, which I have responded to last year in the articles Diet and Exercise: Don’t Do It? and Diet and Exercise: Don’t Do It? Part II. Eating well and exercising—although benefits are not the same for each individual (and I do not know who made the claim this was the case)—does ameliorate numerous diseases and can extend lifespan, contrary to the results of certain studies (e.g., the Look AHEAD study; Annuzzi et al 2014).
Claims from people like JayMan who do not know the first thing about dieting and exercise are dangerous—though, all one has to do is have a basic understanding of physiology to understand that the claim “a fair fraction of people respond little to even *negatively* to exercise” is false, since everyone who does something for the first few times will ALWAYS be better in the months after learning the specific movement, implying that there are no nonresponders to exercise.
Of course everyone does not respond the same to exercise regimen A. Other studies found that increasing the frequency, reps, and set scheme lead to changes in the so-called “nonresponders.” Different individuals respond differently to different training programs [be it, strength, conditioning, cardio, plyometrics, balance, and stabilization etc. But it must be stressed that, although not everyone has the same potential for muscle-building/strength-gaining as, say, the IFBB pros or strongmen/powerlifters, everyone can and does benefit from NOT being sedentary, that much is most definitely clear. These studies that show “nonresponders” run people through the same exercise regimen. Anyone with an iota of experience in this industry knows that people do not respond the same to any and every exercise regimen and, so, the program must be tailored to that specific individual. Though, people like JayMan read this stuff and, without understanding what they’re talking about, jump to brash conclusions that are not supported by reality.
Racial Differences in Physical Functioning
1350 words
Assessing physical functioning is important. Such simple tests—such as walk, stand, and sit tests—can predict numerous things. “Testing” defines one’s abilities after being given a set of instructions. Racial differences exist and, of course, both genetic and environmental factors play a part in health disparities between ethnies in America. Minorities report lower levels of physical activity (PA) than whites, this—most often—leads to negative outcomes, but due to their (average) physiology, they can get away with doing “less” than other ethnies. In this article, I will look at studies which talk about racial differences in physical functioning, what it means, and what can be done about it.
Racial differences in physical functioning
Racial differences in self-rated health at similar levels of health exist (Spencer et al, 2009). Does being optimistic or pessimistic about health effect one’s outcomes? Using 2,929 HABC (Health, Aging, and Body Composition) participants, Spencer et al (2009) examined the relationship between self-rated health (SRH) and race, while controlling for demographic, psychosocial and physical health factors. They found that whites were 3.7 times more likely than blacks to report good SRH.
Elderly blacks were more likely to be less educated, reported lower satisfaction with social support, and also had lower scores on a physical battery test than whites. Further, black men and women were less likely to report that walking a quarter mile was “easy”, implying that (1) they have no endurance and (2) weak leg muscles.
Blacks were also more likely to report higher personal mastery:
Participants were asked whether they agreed or disagreed with the following statements: “ I often feel helpless in dealing with the problems of life ” and “ I can do just about anything I really set my mind to do, ” with response categories of disagree strongly, disagree somewhat, agree somewhat, and agree strongly. (Spencer et al, 2009: 90)
Blacks were also more likely to report higher BMI and more chronic health conditions than whites. White men, though, were more likely to report higher global pain, but were older than black men in the sample. When whites and blacks of similar physical functioning were compared, whites were more likely to report higher SRH. Health pessimists were found to be at higher risk of poor health.
Vazquez et al (2018) showed that ‘Hispanics’ were less likely to report having mobility limitations than whites and blacks even after adjustment for age, gender, and education. Blacks, compared to non-‘Hispanic’ whites were more likely to have limitations on activities of daily living (ADL) and instrumental activities of daily living (IADL) For ADL limitations, questions like “Do participant receive help or supervision with personal care such as bathing, dressing, or getting around the house because of an impairment or a physical or mental health problem?” and for IADLs “Does participant receive help or supervision using the telephone, paying bills, taking medications, preparing light meals, doing laundry, or going shopping?” (Vazquez et al, 2018: 4). They also discuss the so-called “Hispanic paradox” (which I discussed), but could not come to a conclusion on the data they acquired. Nonetheless, ‘Hispanic’ participants were less likely to report mobility issues; blacks were more likely than whites to report significant difficulties with normal activities of daily living.
Araujo et al (2010) devised a lower-extremities chair test: how quickly one can stand and sit in a chair; along with a walking test: the time it takes to walk 50 feet. Those who could not complete the chair test were given a score of ‘0’. Overall, the composite physical function (CPF) score for blacks was 3.45, for ‘Hispanics’ it was 3.66, and for whites, it was 4.30. This shows that older whites were stronger—in the devised tests—and that into older age whites are more likely to not need assistance for everyday activities.
This is important because differences in physical functioning between blacks and whites can explain differences in outcomes one year after having a stroke (Roth et al, 2018). This makes sense, knowing what we know about stroke, cognitive ability and exercise into old age.
Shih et al (2005) conclude:
a nationally representative study of the US population, indicate that among older adults with arthritis: (1) racial disparities found in rates of onset of ADL [activities of daily living] limitations are explained by differences in health needs, health behaviors, and economic resources; (2) there are race-specific differences in risk factors for the onset of ADL limitations; and (3) physical limitations are the most important risk factor for onset of ADL limitations in all racial and ethnic groups.
Safo (2012) showed that out of whites, blacks and “Hispanics”, blacks reported the most (low back) pain, worse role functioning score and overall physical functioning score. Lavernia et al (2011) also found that racial/ethnic minorities were more likely to report pain and have lower physical functioning after having a total knee arthroplasty (TKA) and total hip arthroplasty (THA). They found that blacks and ‘Hispanics’ were more likely to report pain, decreased well-being, and have a lower physical functioning score, which was magnified specifically in blacks. Blacks were more likely to report higher levels of pain than whites (Edwards et al, 2001; Campbell and Edwards, 2013), while Kim et al (2017) showed that blacks had lower pain tolerance and higher pain ratings. (Read Pain and Ethnicity by Ronald Wyatt.)
Sarcopenia is the loss of muscle tissue which is a natural part of the aging process. Sarcopenia—and sarcopenic obesity (obesity brought on by muscle loss due to aging)—shows racial/ethnic/gender differences, too. “Hispanics” were the most likely to have sarcopenia and sarcopenic obesity and blacks were least likely to acquire those two maladies (Du et al, 2018). They explain why sarcopenic obesity may be higher in ‘Hispanic’ populations:
One possibility to explain the higher rates of sarcopenia and SO in the Hispanic population could be the higher prevalence of poorly controlled chronic disease, particularly diabetes, and other health conditions.
[…]
We were surprised to find that Hispanic adults had higher rates of sarcopenia and SO [sarcopenic obesity]. One possible explanation could be the disparity in mortality rates among ethnic populations. Populations that have greater survival rates may live longer even with poorer health and thus have greater chance of developing sarcopenia. Alternatively, populations which have lower survival rates may not live long enough to develop sarcopenia and thus may identify with lower prevalence of sarcopenia. This explanation appears to be supported by the results of our study and current mortality statistics; NH Blacks have the highest mortality rate, followed by NH Whites, and lastly Hispanics.
Differences in physical activity could, of course, lead to differences in sarcopenic obesity. Physical activity leads to an increase in testosterone in lifelong sedentary men (Hayes et al, 2017), while those who had high physical activity compared to low physical activity were more likely to have high testosterone, which was not observed between the groups that were on a calorie-restricted diet (Kumagai et al, 2016). Kumagai et al (2018) also showed that vigorous physical exercise leads to increases in testosterone in obese men:
We demonstrated that a 12-week aerobic exercise intervention increased serum total testosterone, free testosterone, and bioavailable testosterone levels in overweight/obese men. We suggest that an increase in vigorous physical activity increased circulating testosterone levels in overweight/obese men.
(Though see Hawkins et al, 2008 who show that only SHGB and DHT increased with no increase in testosterone.)
So, clearly, since exercise can increase testosterone levels in obese subjects, and higher levels of testosterone are associated with lower levels of adipose tissue; since adequate levels of steroid hormones are needed for lower levels of adipose tissue (Mammi et al, 2012), then since exercise increases testosterone and higher levels of testosterone lead to lower levels of adipose tissue, if physical activity is increased, then levels of obesity and sarcopenic obesity should decrease in those populations.
Conclusion
Racial differences in physical functioning exist; these differences in physical functioning that exist have grave consequences for certain events, especially after a stroke. Differences in physical functioning/activity cause differences in sarcopenia/sarcopenic obesity in different ethnies. This can be ameliorated by targeting at-risk groups with certain outreach. This type of research shows how differences in lifestyle between ethnies cause differences in physical activity between ethnies as the years progress.
(Also read Evolving Human Nutrition: Implications for Public Health, specifically Chapter 8 on socioeconomic status and health disparities for more information on how and why differences like this persist between ethnies in America.)
Racial Differences in Physical Activity and Acquisition of Coronary Artery Calcification
1200 words
Last week a study was published stating that white men who exercised 3 times the recommendation of 1.5 hours (450 minutes, 7.5 hours) had a higher chance of getting coronary artery calcification (CAC), which is the accumulation of plaque and calcium in the arteries of the heart. You, of course see news headlines such as: “Physically active white men at high risk for plaque buildup in arteries“; “White Men Who Exercise Every Day Have 86 Per Cent Higher Risk of Heart Disease Than Black Men, Study Claims“; “Excessive Exercise May Harm The Heart, Study Suggests “; “Excessive exercise increases risk of arterial plaque buildup in white men“; (and my personal favorite headline about this study): “You can exercise yourself to death, says new study“. People just passing by and reading the title (like most do) may then conclude that “they’re saying not to exercise because of CAC.” No, this is not what they are saying at all.
The Coronary Artery Risk Development in Young Adults (CARDIA) study is one of the most important studies in the study of coronary heart disease that have been undertaken. It is a sample of men and women, about equal numbers of each race, from Birmingham, Alabama; Chicago, Illinois; Minneapolis, Minnesota; and Oakland, California. The study began in 1985-86 and there were follow-up examinations at “1987-1988 (Year 2), 1990-1991 (Year 5), 1992-1993 (Year 7), 1995-1996 (Year 10), 2000-2001 (Year 15), 2005-2006 (Year 20), 2010-2011 (Year 25), and 2015-2016 (Year 30).” The CARDIA website writes:
Data have also been collected on physical measurements such as weight and body composition as well as lifestyle factors such as dietary and exercise patterns, substance use (tobacco and alcohol), behavioral and psychological variables, medical and family history, and other chemistries (e.g., insulin).
So there is a goldmine of information to be gleaned from this data. The study that is getting press in the news uses data from this cohort.
The study
The study is titled 25-Year Physical Activity Trajectories and Development of Subclinical Coronary Artery Disease as Measured by Coronary Artery Calcium by Laddu et al (2017). They studied three cohorts by the amount of time they exercised per week: below requirement, at requirements, or above requirements. It is recommended to exercise at least 150 minutes per week.
There were 3,175 men and women who participated in the CARDIA study between 1985 and 2011 who had CAC data available for 25 years. About 47.4 percent of the sample was black, with 56.6 being women. The cohort “consisted of 18.9% black men, 24.6% white men, 28.6% black women, and 28.0% white women” (Laddu et al, 2017).
Of the three activity levels they studies (below 150 minutes, 150 minutes, and over 150 minutes), they observed that white men who exercised 3 times the weekly recommendation (150 minutes(3)= 450 minutes=7.5 hours) had a higher chance of developing CAC. It’s worth noting that exercise time was self-reported (which is the only way I can see how something like this would work, are you supposed to follow people with a camera every day to see how long they engage in physical activity?).
In regards to the physical activity measurement, Laddu et al (2017) write:
At each of the 8 examinations, self-reported leisure-time PA was ascertained by the interviewer-administered CARDIA Physical Activity History Questionnaire.17 Participants were asked about the frequency of participation in 13 specific categories (8 vigorous intensity and 5 moderate intensity) of recreational sports, exercise, home maintenance, and occupational activities during the previous 12 months. Intensity for each activity was expressed as metabolic equivalents (METs), in which 1 MET is defined as the energy expended at rest, which is approximately equivalent to an oxygen consumption of 3.5 mL per 1 kg of body weight per minute.18Vigorous activities (≥6 METs) included running or jogging; racquet sports; biking; swimming; exercise or dance class; job lifting, carrying, or digging; shoveling or lifting during leisure; and strenuous sports. Moderate-intensity activities (3-5 METs) included nonstrenuous sports, walking and hiking, golfing and bowling, home exercises or calisthenics, and home maintenance or gardening.19 Each activity was scored according to whether it was performed for 1 hour or longer during any 1 month during the past year, the number of months it was performed at that level, and the number of months the activity was performed frequently. Each activity was then assigned an intensity score, ranging from 3 to 8 METs, and a duration threshold (ranging from 2-5 hours per week), above which participation was considered to be frequent.20
This is a good metric; though I would like to see a study that looks at just gym-going activity and death, time spent in the gym strength training/moderate to intense cardio. Nevertheless, white men who reported more physical activity had a higher chance of acquiring CAC. Though I can see people’s recall being hazy, people over/under reporting, etc etc.
White men who exercised 7.5 hours per week were 27 percent more likely to get CAC, whereas blacks who exercised that much were at no greater risk to acquire CAC when compared to whites (7.5 hours of exercise compared to less than 2.5 hours per week). Black women who exercised less than the recommendations had a higher chance of acquiring CAC. The researchers couldn’t ascertain why white men who exercised three times the recommendations had such a higher chance of acquiring CAC by the time they reached middle age, but Dr. Jamal Rana says “however this plaque buildup may well be of the more stable kind, and thus less likely to rupture and causes heart attack, which was not evaluated in this study.” The head author, Dr. Deepika Laddu also reiterated: “it does not suggest that anyone should stop exercising.” So people who just read these click bait headlines who say “They’re telling whites not to exercise!”, you’re wrong and you should read papers and not news articles.
This is the perfect example of people reading click baity, fear-mongering headlines and running with it. I saw some people saying “They’re telling us not to exercise!” No. If you were to read the paper and any serious news articles on the matter, you’d see that they do not recommend that people do not exercise. Now the question is, why do whites who exercise more than 7.5 hours per week have a higher chance of acquiring heart disease? I can think of a few explanations (though they are not satisfactory): 1) genes: which genes? Why? How do they interact with the body over time to lead to arterial calcification?; 2) dietary habits: I’d like to know what their diet was like and see their macro composition, carbohydrates, not saturated fat, causes heart disease (Siri-Tirino et al, 2010; de Souza et al, 2015) so that may be a huge contributing factor.
Nevertheless, this is yet another physiological race difference. Oddly enough, black men are more likely than white men to have hypertension (Hicken et al, 2013).
Even though black men, on average, have higher rates of hypertension than white men, white men who are physically active for 7.5 had a higher chance of acquiring CAC than those who exercised less than 2.5 hours per week. This effect wasn’t seen in black men who had physical activity at that level, which, of course, implies that differences in genes and SES underlie this difference. I await more papers into this matter into the mechanisms of how and why this occurs and will ruminate on this myself in the future. No, this study does not tell white men not to exercise.
Diet and Exercise: Don’t Do It?
1800 words
On Twitter, JayMan linked to a video about a time traveling dietician who travels back to the 70s to give nutritional advice to a couple. He kept going back on what he said, re eggs and cholesterol, Paleo diet, etc. Then at the end of the video, the ‘time traveling dietician’ says “It turns out it’s genetic. It doesn’t matter whether you exercise or what you eat.”
I then asked JayMan if he was advising people to not diet or exercise—and if he was doing so—what credentials does he have to give such advice? “Appeal to authority!” So if some random guy gave me legal advice and I asked his credentials, is that an appeal to authority? Similarly, if someone is trying to give me medical advice, is asking where he got his medical license an appeal to authority? The thing is, people have specialties for a reason. I wouldn’t take diet and exercise advice from some anon blogger with no credentials, just like I wouldn’t take legal advice from a biologist. Anyway, I’ll review some studies on exercise, dieting, and sitting in regards to all-cause mortality.
Sitting and all-cause mortality
Listening to such advice—like not dieting or exercising—will lower your quality of life and life expectancy. The longer you sit, the more likely you are to have rolled shoulders among other postural imbalances. One of the biggest reasons that sitting is related to all-cause mortality (Chau et al, 2013; Biddle et al, 2016). So listening to this shitty advice to ‘not exercise’ will lead an individual to having a lower QoL and lower life expectancy.
Sitting is associated with all-cause mortality because if, say, one is sitting at a desk for 8 hours per day then goes home and sits for the rest of the day, circulation will not get not get to the lower extremities. Furthermore, even mild-to-moderate exercise attenuates the situation (Chau et al, 2013). Further, reducing sedentary behavior (and of course, watching less TV) can possibly raise life expectancy in the US (Katzmarzyk and Lee, 2012). They found that cutting daily sitting time to less than three hours can increase life expectancy by two years (and, of course, quality of life). There is a large body of research on sitting and all-cause mortality (Stamatakis et al, 2013). It’s also worth noting that too much sitting decreases life expectancy—even with exercise. So JayMan’s (unprofessional) advice will lead to someone having a shitty life quality and lower life expectancy.
Dieting, and all-cause mortality
This is a bit trickier. I know that dieting for weight loss doesn’t work (Aamodt, 2016; Fung, 2016)—that is, traditional dieting (high-carb diets). The traditional advice is to eat high-carb, low-fat and moderate protein—this is due to what occurred in the 70s—the demonization of fat and the championing of carbs. This, clearly, is wrong. This has led to the obesity epidemic and the cause is our evolutionary novel environments. The main reason is that we have constructed environments for ourselves that are novel, and thus we’ve not had enough time to adapt to what we eat/how we live our new lives in our modernized world.
Indeed, even hunter-gathers don’t have our disease rates that we have—having low to no cases of our diseases of civilization (see Taubes, 2007 for a review). Why is this? It’s because they are physically active and they do not eat the same processed carbohydrates that we in first-world societies do.
In regards to exercise and all-cause mortality, people who exercise more often have a lower chance of dying from all causes than more sedentary people (Oja et al, 2016; O’Donovan et al, 2017). So it’s becoming clear that JayMan is just talking out out his ass here. I’d love to hear any MD say to a patient “Don’t diet, don’t exercise. Don’t eat well. It doesn’t work.” Because that MD will be a shill for Big Food.
Further, when I say ‘diet’, I don’t mean eating below the BMR. Your ‘diet’ is what you eat, and by changing your diet, you’re changing to healthier habits and eating higher-quality foods. People like JayMan make it seem like you should eat whatever you want and not to exercise. Following this advice, however, will lead to deleterious consequences.
It DOES matter what you put into your body; it DOES matter if you exercise or not. If you do not, you will have a lower life expectancy than who does exercise and eats well.
On a side note, I know that dieting does not work for weight loss. Traditional dieting, that is. Dr. Jason Fung, world-renowned obesity, diabetes and intermittent fasting expert, has people lose and keep their weight off. He actually understands what causes obesity—insulin. Higher insulin levels are also tied to the obesity pathway through lack of glucagon receptors (Lee et al, 2014). Why is this important? First, we have to understand what insulin does in the body. Once you understand what insulin does in the body then you will see why JayMan is wrong.
Insulin inhibits the breakdown of fat in the adipose tissue by inhibiting the lipase that hydrolyzes (the chemical breakdown of a compound due to a reaction with water) the fat out of the cell. Since insulin facilitates the entry of glucose into the cell, when this occurs, the glucose is synthesized into glycerol. Along with the fatty acids in the liver, they both are synthesized into triglycerides in the liver. Due to these mechanisms, insulin is directly involved with the shuttling of more fat into the adipocyte. Since insulin has this effect on fat metabolism in the body, it has a fat-sparing effect. Insulin drives most cells to prefer carbohydrates for energy. Putting this all together, insulin indirectly stimulates the accumulation of fat into the adipose tissue.
Does this physiologic process sound that you can ‘eat whatever you want’? Or does it tell you that you should lower your carb intake as to not induce blood glucose spikes which lead to an increase in insulin? Over time, these constant blood glucose/insulin spikes lead to insulin resistance which has the body produce more insulin due to the insulin resistance resulting in a vicious cycle.
So, it seems that in order to have a higher QoL and life expectancy, one must consume processed carbs very sparingly.
These behaviors of over consuming processed carbohydrates come down to the environments we have constructed for ourselves—obesogenic environments. An obesogenic environment “refers to an environment that helps, or contributes to,
obesity” (Powell, Spears, and Rebori, 2010).
Our current obesogenic environment also contributes to dementia and cognitive impairment. What makes environments ‘obesogenic’ “is the increased presence of food cues and the increased consumption of a diet which compromises our ability to resist those cues” (Martin and Davidson, 2015). So if our obesogenic environments change, then we should see a reduction in the number of overweight/obese people.
Diet is very important for Type II diabetics. For instance, TII diabetics can manage, and even reverse, their disease with a low-carb ketogenic diet (LCKD) lowering their hBA1c, having a better lipid profile, cardiac benefits, weight loss etc (Westman et al, 2008; Azar, Beydoun, and Albadri, 2016; Noakes and Windt, 2016; Saslow et al, 2017). I wonder if JayMan would tell TII diabetics not to diet or exercise…. That’d be a recipe for disaster. TII diabetics need to keep their insulin down and eating an LCKD will do that; taking JayMan’s ‘advice’ not to diet or exercise will quickly lead to more weight gain, an exacerbation of problems and, eventually, death due to complications from not correctly managing the disease. JayMan needs to learn the literature and understand these papers to truly understand why he is wrong.
Exercise and all-cause mortality
The relationship between vigorous exercise and all-cause mortality is well studied. Gebel et al (2015) conclude that “Independent of the total amount of physical activity, engaging in some vigorous activity was protective against all-cause mortality. This finding applied to both sexes, all age categories, people with different weight status, and people with or without cardiometabolic disease.” Reduced exercise capacity also causes higher all-cause mortality rates (McAuley et al, 2016).
Unfit thin people had two times higher mortality rate than normal weight fit people. Further, overweight and obese fit people had similar mortality rates when compared to normal weight fit people (Barry et al, 2013). Clearly, physical activity needs to be heightened if one wants to live a longer, higher quality life. This runs completely opposite of what JayMan is implying.
Exercise into old age is also related to higher cognition and lower mortality rate in when compared to individuals who do not exercise. Exercise also protects against cognitive degeneration in the elderly (Bherer, Erikson and Lie-Ambrose, 2013; Carvalho et al, 2014; Paillard, 2015). If you want to keep your cognition into old age and live longer, it seems like your best bet is to exercise at a young age in order to stave off cognitive degeneration.
Strength and mortality
Finally, one last thing I need to touch on is strength and mortality. Strength is, obviously, increased through exercise. Stronger men live longer—and are protected from more disease such as cancer—than weaker men, even when controlling for cardiorespiratory fitness and other confounds (Ruiz et al, 2008).
As I have covered in the past, differences in grip strength account for differences in mortality in men—which also has a racial component (Araujo et al, 2010; Volkalis, Halle, and Meisinger, 2015). The stronger you are, the less chance you have of acquiring cancer and other maladies. Does the advice of ‘don’t exercise’ sound good now? It doesn’t, and I don’t know why anyone would seriously imply that dieting and exercise doesn’t work.
Conclusion
Dieting (meaning eating a higher quality diet, not attempting to lose weight) and exercise do work to increase life expectancy. The advice of “don’t do anything, it’s genetic” makes no sense at all after one sees the amount of literature there is on eating mindfully and exercising. I know that exercise does not induce weight loss, but it does contribute to living longer and staving off disease.
People should stay in their lane and leave things to the professionals—the people who are actually working with individuals every day and know and understand what they are going through. The canard of ‘eat whatever, don’t exercise, it’s genetic’ is very dangerous, especially today when obesity rates are skyrocketing. JayMan needs to learn the literature and how and why exercise and eating right leads to a higher quality of life and life expectancy. Thankfully, people like JayMan who say not to diet or exercise have no pull in the real world.
Clearly, to live longer, eat right, don’t sit for too long (because even if you exercise, sitting too long will lower your life expectancy) and exercise into old age and your chance of acquiring a whole slew of deleterious diseases will be lessened.