Not Feeling Pain: What is CIPA (Congenital Insensitivity to Pain with Anhydrosis)?
1750 words
“Congenital Insensitivity to Pain” (CIPA, or congenital analgesia: CIPA hereafter) is an autosomal recessive disease (Indo, 2002) and was first observed in 1932 (Daneshjou, Jafarieh, and Raeeskarami, 2012). It is called a “congenital disorder” since it is present from birth. Since the disease is autosomal recessive, the closer the two parents are in relatedness, the more likely it is they will pass on a recessive disorder since they are more likely to have and pass on autosomal recessive mutations (Hamamy, 2012). First cousins, for example, 1.7-2.8% higher risk of having a child with an autosomal recessive disease (Teeuw et al, 2013). Consanguinity is common in North Africa (Anwar, Khyatti, and Hemminki, 2014) and the Bedouin have a high rate of this disease (Schulman et al, 2001; Lopez-Cortez et al, 2020; Singer et al, 2020). Three mutations in the TrkA (AKA NTRK1) have been shown to induce protein mis-folding which affect the function of the protein. Different mutations in the TrkA gene have been shown to have be associated with different disease outcomes (Franco et al, 2016). Since the mutated gene in question is needed for nerve growth factors, the pain signals cannot be transferred to the brain since there are hardly any of them there (Shin et al, 2016).
Individuals unfortunate enough to be inflicted with CIPA cannot feel pain. Whether it’s biting their tongues, feeling pain from extreme temperatures. People with CIPA have said that while they can feel the difference between extreme temperatures—hot and cold—they cannot feel the pain that is actually associated with the temperatures on their skin see (Schon et al, 2018). When they bump into things, they may not be aware of what happened and injuries may occur which heal incorrectly due to no medical attention and only noticing the fractures and other things that occur due to CIPA years later after they see doctors for what is possibly factors due to having the disease. People with CIPA are thought to be “dumb” because they constantly bump into things. But what is really happening is that, since they cannot feel pain, they have not learned that bumping into things could be damaging to their bodies, as pain is obviously an experience-dependent event. So these people learn, throughout their lives, to fake being in pain as to not draw suspicion to people who may not be aware of the condition. Children with the disease are thought, most of the time, to be victims of child abuse, but when it is discovered that the child who is thought to be a victim of abuse is inflicted with CIPA (van den Bosch et al, 2014; Amroh et al, 2020), treatments shift toward managing the disease.
About twenty percent of people with CIPA live until three years of age (Lear, 2011), while 20 percent of those who die at age 3 die from complications due to hyperpexia (an elevated body temperature over 106. degrees Fahrenheit) (Rosemberg, Marie, and Kliemann, 1994; Schulmann et al, 2001; Indo, 2002; Nabyev et al, 2018). Since they cannot feel the heat and get themselves to cool down, Due to a low life expectancy (many more live until about 25 years of age), this disease is really hard to study (Inoyue, 2007; Daneshjou, Jafarieh, and Raeeskarami, 2012). People hardly make it past that age since they either don’t feel the pain and do things that normal people, through experience, know not to do since we can feel pain and know to not do things that cause us pain and discomfort or they commit suicide since they have no quality of life due to damaged joints. Furthermore, since they cannot feel pain, people with this disease are more likely to self-mutilate since they cannot learn that self-mutilation causes pain (since pain is a deterrent for future action that may in fact cause pain to an individual). They also cannot sweat, meaning that control of the body temperature of one afflicted with CIPA is of utmost precedence (since they could overheat and die). Thus, these cases of deaths of individuals with CIPA do not occur due to CIPA per se, they occur due to, say, not feeling heat and then sweating while not attempting to regulate their body temperature and cool down (whether by naturally sweating due to being too hot or getting out of the extreme hot temperature causing the elevated body temperature). This is known as “hyperpyrexia” and this cause of death affects around 20 percent of CIPA patients (Sasnur, Sasnur, and Ghaus-ul, 2011). Furthermore, they are more likely to have thick, leathery skin and also show little muscular definition.
Not sweating is associated with CIPA and if one cannot sweat, one cannot have their body temperature regulated when they get too hot. So if they get too hot they cannot feel it and they will die of heat stroke. The disease, though, is rare, as only 17-60 people in America currently have it, while there are about 600 cases of the disease worldwide (Inoyue, 2007; Lear, 2011). This disease is quite hard to identify, but clinicians may be able to detect the presence of the disease through the following ways: Infants biting their lips, fingers, cheeks and not crying or showing any instance of being in pain after the event; repeated fractures in older children; a history of burns with no medical attention; observing that a child has many healed joint injuries and bone fractures without the child’s parents seeking medical care; observing that the patient does not react to hot or cold events (though they can say they can feel a difference between the two) they make errors in distinguishing in whether something is hot or cold (Indo, 2008).
Children who have this disease are at a higher risk of having certain kinds of bodily deformations, since they cannot feel the pain that would make them be hesitant to perform a certain action in the future. Due to this, people with this disease must constantly check themselves for cuts, abrasions, broken bones, etc to ensure that they cannot feel when they actually occur to them. They don’t cry, or show any discomfort, when experiencing what should be an event that would cause someone without CIPA to cry. CIPA-afflicted individuals are more likely to have bodily deformations since their joints and bones do not heal correctly after injury. This then leads to their walking and appearance to be affected. This is one of many reasons why the parents of people with CIPA must constantly check their children for signs of bodily harm or unintentional injuries. One thing that needs to be looked out for is what is termed Charcot joint—which is a degenerative joint disorder (Gucev et al, 2020).
A specific form of CIPA—called HSAN-IV—was discovered in a village in southern Finland called Vittangi, where it was traced to the founder of the village itself in the 1600s. Since the village was remote with such a small population, this meant that the only people around to marry and have children with were people who were closely related to each other. This, then, is the reason why this village in Finland has a high rate of people afflicted with this disease (Norberg, 2006; Minde, 2006). This, again, goes back to the above on consanguinity and autosomal recessive diseases—since CIPA is an autosomal recessive disease, one would reason that we would find it in populations that marry close relatives, either due to custom or population density.
Many features have been noted as showing that an individual is afflicted with CIPA: absent pain sensation from birth, the inability to sweat; and mental retardation, lower height and weight for their age (Safari, Khaledi, and Vojdani, 2011; Perez-Lopez et al, 2015). Children with CIPA have lower IQs than children without CIPA, so there is an inverse relationship between IQ and age; the older the age of the child with CIPA, the lower their IQ, while the reverse is true for individuals who are younger (Erez et al, 2010). One girl, for example. had a WISC-III IQ of 49, and she self-mutilated herself by picking at her nails until they were no longer there (Zafeirou et al, 2004). Another girl with CIPA was seen to have an IQ of 52, be afflicted with mental retardation, have a low birth weight, and was microcephalic (Nolano et al, 2000). Others were noted to have IQs in the normal range (Daneshjou, Jafarieh, and Raaeskarami, 2012). People with a specific form of this disease (HSN type II) were observed to have IQs in the normal range (though it is “caused by” a different set of genes than CIPA, HSN type IV; Kouvelas and Terzoglou, 1989). However, it has been noted that the cut-off of 70 for mental retardation is arbitrary (see Arvidsson and Granlund, 2016). While running a full gamut of tests on an individual thought to have CIPA, we can better attempt to ensure a higher quality of life in individuals afflicted with the disease. In sum, IQ scores of CIPA individuals do not reflect that the mutations in TrkA “cause” IQ scores; it is an outcome of a disrupted system (in this case, mutations on the TrkA gene).
There is currently no cure for this disease, and so, the only way to manage complications stemming from CIPA is to work on the injuries that occur to the joints that occur as they happen, to ensure that the individual has a good quality of life. Treatment for CIPA, therefore, is not actually curing the disease, but it is curing what occurs due to the disease (bone breaks, joint destruction), which would then heighten the quality of life of the person with CIPA (Nabiyev, Kara, and Aksoy, 2016). Naloxone may temporarily relieve CIPA (Rose et al, 2018), while others suggest treatments such as remifentanil (Takeuchi et al, 2018). We can treat outcomes that arise from the disease (like self-mutilation), but we cannot outright cure the disease itself (Daneshjou, Jafarieh, and Raaeskarami, 2012). The current best way to manage the disease is to identify the disease early in children and to do full-body scans of afflicted individuals to attempt to cure the by-products of the disease (such as limb/joint damage and other injuries). Maybe one day we can use gene therapy to help the afflicted, but for now, the best way forward is early identification along with frequent check-ups. By managing body temperature, having frequent check-ups, modifying the behavior of the child as to avoid injuries, wearing a mouth guard so they do not grind their teeth or bite their tongue, avoiding hot or cold environments or food, (Indo, 2008; Rose et al, 2018).
CIPA is a very rare—and very interesting—disease. By better understanding its aetiology, we can better help the extremely low number of people in the world who suffer from this disease.
Racial Differences in Amputation
1850 words
Overview
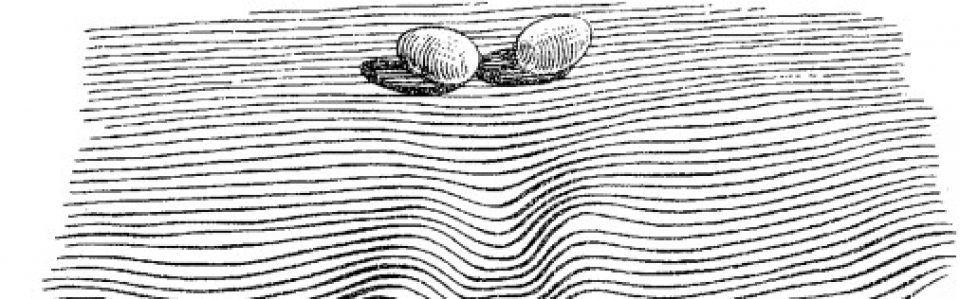
An amputation is a preventative measure. It is done for a few reasons: To stop the spread of a gangrenous infection and to save more of a limb after there is no blood flow to the limb after a period of time. Other reasons are due to trauma and diabetes. Trauma, infection, and diabetes are leading causes of amputation in developing countries whereas in developed countries it is peripheral vascular disease (Sarvestani and Azam, 2013). Poor circulation to an affected limb leads to tissue death—when the tissue begins turning black, it means that there is no or low blood flow to the tissue, and to save more of the limb, the limb is amputated just above where the infection is. About 1.8 million Americans are living as amputees. After amputation, there is a phenomenon called “phantom limb” where amputees can “feel” their limb they previously had, and even feel pain to it, and it is very common in amputees; about 60-80 percent of amputees report “feeling” a phantom limb (see Collins et al, 2018; Kaur and Guan, 2018). The sensation can occur either immediately after amputation or years after. Phantom limb pain is neuropathic pain—a pain that is caused by damage to the somatosensory system (Subedi and Grossberg, 2011). Amputees even have shorter lifespans. When foot-amputation is performed due to uncontrolled diabetes, mortality ranges between 13-40 percent for year one, 35-65 percent for year 3, and 39-85 percent in year 5 (Beyaz, Guller, and Bagir, 2017).
Race and amputation
Amputation of the lower extremities are the most common amputations (Molina and Faulk, 2020). Minority populations are less likely to receive preventative care, such as preventative vascular screenings and care, which leads to them being more likely to undergo amputations. Such populations are more likely to suffer from disease of the lower extremities, and it is due to this that minorities undergo amputations more often than whites in America. Minorities in America—i.e., blacks and “Hispanics”—are about twice as likely as whites to undergo lower-extremity amputation (Rucker-Whitaker, Feinglass, and Pearce, 2003; Lowe and Tariman, 2008; Lefebvre and Lavery, 2011; Mustapha et al, 2017; Arya et al, 2018)—so it is an epidemic for black America. Blacks are even more likely to undergo repeat amputation (Rucker-Whitaker, Feinglass, and Pearce, 2003). In fact, here is a great essay chronicling the stories of some double-amputee black patients.
Why do blacks undergo amputations more often than whites? One answer is, of course: Physician bias. For example, after controlling for demographic, clinical, and chronic disease status, blacks were 1.7 times more likely than whites to undergo lower-leg amputations (Feinglass et al, 2005; Regenbogen et al, 2007; Lefebvre and Lavery, 2011). What is a cause of this is inequity in healthcare—note that “inequity” here means differences in care that are avoidable and unjust (Sudana and Blas, 2013).
Another reason is due to complications from diabetes. Blacks have higher rates of diabetes than whites (Rodriguez and Campbell, 2007) but see Signorello et al (2007). Muscle fiber differences between races (see also here). Differences in hours-slept between blacks and whites, too, could also explain the severity of the disease. But what could also be driving differences in diabetes between races is the fact that blacks are more likely than whites to live in “food swamps.” Food swamps are where it is hard to find nutritionally-dense food, whereas food deserts are areas where there is little access to healthy, nutritious food. In fact, a neighborhood being a food swamp is more predictive of obesity status of the population in the area than is its being a food desert (Cooksey-Stowers, Schwartz, and Brownell, 2017). Along with the slew of advertisements in that are directed to low-income neighborhoods (see Cassady, Liaw, and Miller, 2015), we can now see how such things like food swamps contribute to high hospitalization rates in low-income neighborhoods (Phillips and Rogriguez, 2019). These amputations are preventable—and so, we can say that there is a lack of equity in healthcare between races which leads to these different rates in amputation—before even thinking about physician bias. Amputation rates for blacks in the southeast can be almost seven times higher than other regions (Goodney et al, 2014).
Stapleton et al (2018: 644) conclude in their study on physician bias and amputation:
Our study demonstrates that such justifications may be unevenly applied across race, suggesting an underlying bias. This may reflect a form of racial paternalism, the general societal perception that minorities are less capable of “taking care of themselves,” even including issues related to health and disease management.23 Underlying bias may prompt more providers to consider amputation for minority patients. Furthermore, unlike in transplant surgery, there is currently no formal process for assessing patient compliance with treatment protocols or self-care in vascular surgery.24 Asking providers to make snap judgments about patient compliance, without a protocol for objective assessment, allows subconscious bias to influence patient care.
Physician bias is pervasive (Hoberman, 2012)—whether it is conscious or unconscious racial bias. Such biases can and do lead to outcomes that should not occur. By attempting to reduce disparities in healthcare that then lead to negative outcomes, we can then attempt to improve the quality of healthcare given to lower-income groups, like blacks. Such biases lead to negative health outcomes for blacks (such as the claim that blacks feel less pain than whites), and if they were addressed and conquered, then we could increase equity between groups until access to healthcare is equal—and physician bias is an impediment to access to equal healthcare due to the a priori biases that physicians may hold about certain racial/ethnic groups. Medical racism, therefore, drives a lot of the amputation differences between blacks and whites. Hospitals that are better equipped to offer revascularization services (attempting to save the limb by increasing blood flow to the affected limb) even had a higher rate of amputations in blacks when compared to whites (Durazzo, Frencher, and Gusberg, 2013).
For example. Mustapha et al (2017) write:
Compared to Caucasian patients, several studies have found that African-Americans with PAD are more likely to be amputated and less likely to have their lower limb revascularized either surgically or via an endovascular approach [3–9]. In an early analysis of data from acute-care hospitals in Florida, Huber et al. reported that the incidence of amputation (5.0 vs. 2.5 per 10,000) was higher and revascularization lower (4.0 vs. 7.1 per 10,000) among African-Americans compared to Caucasians, even though the incidence of any procedure for PAD was comparable (9.0 vs. 9.6 per 10,000) [4]. Other studies have reported that the probability of undergoing a revascularization or angioplasty was reduced by 28–49 % among African-Americans relative to Caucasians [3 6]
Pro-white unconscious biases were also found among physicians, as Kandi and Tan (2020) note:
There is evidence of both healthcare provider racism and unconscious racial biases. Green et al. found significant pro-White bias among internal medicine and emergency medicine residents, while James SA supported this finding, indicating a “pro-white” unconscious bias in physician’s attitudes towards, and interactions with, patients [43,44]. In a survey assessing implicit and explicit racial bias by Emergency Department (ED) providers in care of NA children, it was discovered that many ED providers had an implicit preference for white children compared to those who identified as NA [45]. Indeed, racism and stigmatization are identified as being many American Indians’ experiences in healthcare.
One major cause of the disparity is that blacks are not offered revascularization services at the same rate as whites. Holman et al (2011: 425) write:
Finally, given that patients’ decisions are necessarily confined to the options offered by their physicians, racial differences in limb salvage care might be attributable to differences in physician decision making. There are some data to suggest lower vein graft patency rates in black patients compared to whites.18,19 A patient’s race, therefore, may influence a vascular surgeon’s judgment about the efficacy of revascularization in preventing or delaying amputation. Similarly, a higher proportion of black patients in our sample were of low SES, which correlates with tobacco use,20-22 and we know that continued tobacco use increases the risk of lower extremity graft failure approximately three-fold.23 It is possible that a higher proportion of black patients in our sample were smokers who refused to quit, in which case vascular surgeons would be much less likely to offer them the option of revascularization. While Medicare data include an ICD-9 diagnosis code for tobacco use, the prevalence in our study sample was approximately 2%, suggesting that this code was grossly unreliable as a means of directly measuring and adjusting for tobacco use.
Smoking, of course, could be a reason why revascularization would not be offered to black patients. Though, as I have noted, smoking ads are more likely to be found in lower-income neighborhoods which increases the prevalence of smokers in the community.
With this, I am reminded of two stories I have seen on television programs (I watch Discovery Health a lot—so much so that I have seen most of the programs they show).
In Untold Stories of the ER, a man came in with his hand cut off. He refused medical care. He would not let the doctors attempt to sew his hand back on. Upon the police entering his home to check for evidence (where his hand was found), they searched his computer. It seems that he had a paraphilia called “acrotomophilia” which is where one is sexually attracted to people with amputations. Although he wanted it to be done to himself—he had inflicted the wound on himself. After the doctor tried to reason with the man to have his hand sewed back on, the man would not let up. He did not want his hand sewed back on. I wonder if, years down the line, the man regretted his decision.
In another program (Mystery Diagnosis), a man had said that as a young boy, he had seen a single-legged war veteran amputee. He said that ever since then, he would do nothing but think about becoming an amputee. He lived his whole life thinking about it without doing anything about it. He then went to a psychiatrist and spoke of his desire to become an amputee. After some time, he eventually flew to Taiwan and got the surgery done. He, eventually, found happiness since he had done what he always wanted to.
While these stories are interesting they speak to something deep in the minds of the individuals who mutilate themselves or get surgery to otherwise healthy limbs.
Conclusion
Blacks are more likely than whites to receive amputations in affected limbs than whites and are less likely to receive treatments that may be able to save the affected limb (Holman et al, 2011; Hughes et al, 2013; Minc et al, 2017; Massada et al, 2018). Physician bias is a large driver of this. So, to better public health, we then must attempt to mitigate these biases that physicians have that lead to these kinds of disparities in healthcare. Medical and other kinds of racism have led to this disparity in amputations between blacks and whites. Thus, to attempt to mitigate this disparity, blacks must get the preventative care needed in order to save the affected limb and not immediately go for amputation. Thankfully, such disparities have been noticed and work is being done to decrease said disparities.
So race is a factor in the decision on whether or not to amputate a limb, and blacks are less likely to receive revascularization services.