Home » Obesity
Category Archives: Obesity
Who Believes in an Afterlife in America? If Heaven Exists, Will There Be Races?
2500 words
(Note: I don’t believe in an afterlife and I’m not a theist.)
What do Americans think about the existence of an afterlife and what are the differences between races?
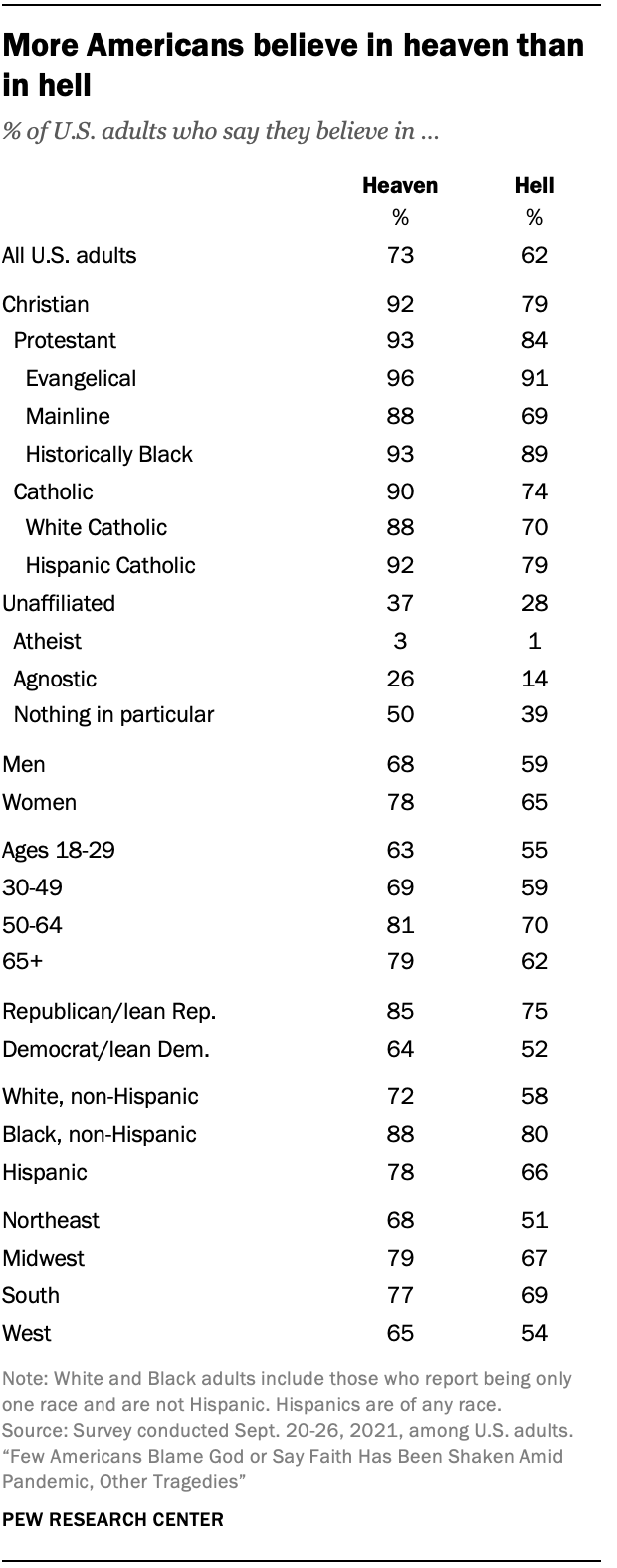
What do Americans think about the existence of an afterlife—of heaven and hell? The existence of an afterlife to American citizens is clear—more Americans believe in heaven but not in hell, per Pew. But 26% of the respondents didn’t believe in either heaven or hell. But those who did not believe in heaven or hell but did believe in an afterlife were asked to describe their views:
Respondents who believe in neither heaven nor hell but do still believe in an afterlife were given the opportunity to describe their idea of this afterlife in the form of an open-ended question that asked: “In your own words, what do you think the afterlife is like?”
Within this group, about one-in-five people (21%) express belief in an afterlife where one’s spirit, consciousness or energy lives on after their physical body has passed away, or in a continued existence in an alternate dimension or reality. One respondent describes their view as “a resting place for our spirits and energy. I don’t think it’s like the traditional view of heaven but I’m also not sure that death is the end.” And another says, “I believe that life continues and after my current life is done, I will go on in some other form. It won’t be me, as in my traits and personality, but something of me will carry on.”
Blacks were slightly more likely to believe in heaven over whites, though a super majority of both races do believe in heaven, while way more blacks than whites believed in the existence of hell. Others professed less-widely-held views on the afterlife, like existing as a spirit, consciousness, or energy in the afterlife. Those who believe state that heaven is free from earthly matters, such as suffering while in hell it is the opposite—hell is nothing but eternal suffering, not due to any fire and brimstone, but because it is eternal separation from God. America is, to my surprise, still a very superstitious country when it comes to God and Satan and the existence of heaven and hell. People believe that their prayers can be answered and that interactions between the living and the dead are possible. Black Americans are more likely to believe that their prayers can be directly answered in comparison to white Americans (83 percent compared to 65 percent, respectively) , while 67 percent of Americans think it’s possible. Black Americans also believe that revelations from a higher power are possible in comparison to white Americans (85 percent and 66 percent, respectively), while black Americans are more likely to believe that they have experienced contact from a higher power compared to white Americans (53 percent compared to 25 percent, respectively).
Blacks are also slightly more likely than whites to believe in near-death experiences (79 percent compared to 73 percent, respectively). Thus, blacks are more superstitious than whites. The Pew poll also tracks other studies—black Americans and Caribbean Blacks were more likely to be religious than whites (Joseph et al, 1996; Franzini et al, 2005; Taylor, Chatters, and Jackson, 2007; Chatters et al, 2009). Men in general are less religious than women, but black men are less religious than black women but more religious than white women. But although blacks are more likely than whites to believe in an afterlife and be religious, there is an apparent shift away (and Americans seem to be shifting away from being religious ever so slightly, though 81 percent of Americans are still believers) from religiosity in the black community; but they are still more likely to pray, say grace and attend church than other racial groups.
Moreover, black men over age 50 who attend church had a 47 percent reduction in all-cause mortality compared to those who did not attend (Bruce et al, 2022), so there seems to be a protective effect that occurs due to attending church services (Assari and Lankarani, 2018; Carter-Edwards et al, 2018; Majee et al, 2022). It has been found that blacks consistently report lower odds of having depression, and the answer is probably due to attending religious services (Reese et al, 2012). However, when it comes to church attendance, for white women their attendance at church is either nonexistent or protective when it comes to body mass while for black women consistent relations between church attendance and body mass have been shown (Godbolt et al, 2018). Given the fact that black women have been consistently more likely to be obese than white women since at least the late 80s and 90s (Gillum, 1987; Kumanyika, 1987; Allison et al, 1997) and today (Tilghman, 2003; Johnson et al, 2012; Agyemang and Powell-Wiley, 2014; Tucker et al, 2021), this finding is not surprising. But the effects of racism can not only explain the higher rates of obesity in black women (Cozier et al, 2014), it could also explain the higher rates of “weathering” of black women’s bodies (Geronimus et al, 2006).
Nevertheless, blacks are more likely to be religious and report religious experiences in comparison to whites, and blacks are also more likely to be religious in comparison to the general US population. Why may blacks be more religious than whites? This is a question I will try to answer in the future.
Is it possible for races to exist in heaven?
Some Christians claim that there will be racial/ethnic diversity in both heaven and hell. The article Will heaven be multicultural and have different races? claims that:
The ultimate answer to your question is found in Revelation 21-22 which describes the new heaven and earth. In Revelation 21:24 we are told that people from the various nations will be in heaven. That is, those who believe in Jesus Christ and follow Him will live there for eternity. But the culture of heaven will be God’s culture. Everything is new. Heaven and earth will be new. The old will have disappeared and the new will have come. Sin will be gone and racial prejudices and alliances will be gone.
While the article Will There Be Ethnic Diversity in Heaven? claims that “ethnic diversity seems to be maintained and apparent in Heaven, for eternity“, the article Racial Diversity in Hell claims that:
The difference between heaven and hell is that in heaven—that is, in the new heaven and new earth—there will be perfect racial and ethnic harmony, but in hell, racial and ethnic animosities will reach their fullest fury and last forever.
So what is RACE? In my view, race is a suite of physical characteristics which are demarcated by geographic ancestry, as argued by Hardimon and Spencer. So if race is physical, then if a thing isn’t physical—that is, if a thing is immaterial—then there would be no way to identify which racial group they were a part of while they were alive. If we take the afterlife to be a situation in which a person has died but they then exist again as a disembodied soul/mind, then there can’t possibly be races in heaven, since what identified the person as part of a racial group (the physical) doesn’t exist anymore.
In the book The Myth of an Afterlife, Drange (2015: 329-330) articulates what he calls the nonidentification argument, where it is inconceivable for a person to be identified if they are bodiless, and if they are bodiless and race is a property of physical bodies, then it would follow that there wouldn’t be races in heaven since disembodied souls, by definition, lack physical bodies—there would be no way for the identities of people to be established, and so if people’s identities cannot be established, then it follows that their racial identities cannot be established either.
- Bodiless people would have no sense organs and no body of any sort.
- Therefore, they could not feel anything by touch or see or hear anything (in the most common senses of “see” and “hear”).
- Thus, if they were to have any thoughts about who they are, then they would have no way to determine for sure that the thoughts are (genuine) memories, as opposed to mere figments of imagination.
- So, bodiless people would have no way to establish their own identities.
- Also, there would be no way for their identities to be established by anyone else.
- Hence, there would be no way whatever for the identities of bodiless people to be established.
- But for a person to be in an afterlife at all, it is conceptually necessary for his or her identity to be capable of being established.
- It follows that a totally disembodied personal afterlife is not conceivable.
Drange’s argument is against a certain conception of the afterlife, mainly if it is one where souls are disembodied, it follows that there would be no way to identify them, and so it follows that there would be no races in heaven, since race is a physical property of humans and their bodies. But there are different ways of looking at the possibility of races in heaven, depending on which theory of race one holds to.
Nathan Placencia (2021) argues that whether or not races exist in heaven depends on which philosophy of race you hold to, but he does make the positive claim that there may be racial identities in heaven. For racial constructivists, since race exists merely due to social conventions and racialization, then race wouldn’t exist. For the racial skeptic, since race doesn’t exist as a biological category, then races don’t exist. That is, since racial naturalism is false, then races of any kind cannot exist, where racial naturalism is basically like the hereditarian conception (or non-conception, if you will) of race (see Kaplan and Winther, 2015). Racial naturalists argue that race is grounded in genetically-mediated biological differences. I am of course sympathetic to the view, though I do hold that race is a social construct of a biological reality and I am a pluralist about race. The last conception that Placencia discusses is that of deflationary realism, where race is genetically-grounded but not itself normatively important (Hardimon, 2017). So Placencia claims that for the racial constructivists and skeptics, races won’t exist in heaven while for the deflationary realist, the “answer is maybe” on whether or not race will exist in heaven which then of course depends on what the resurrected heavenly bodies would look like.
Believers in heaven state that Believers will have new, physical bodies in heaven. But Jesus wasn’t immediately recognizable to his followers, though they did come to know that it was actually him after spending time with him. So theists of course then believe that we get new physical bodies in heaven but that we would look different than we did while we had a physical, earthly existence. Certain chapters in Revelations (21:4, 22:4) talk about God wiping away tears and a name appearing on their foreheads, so this then implies that there would be new, physical bodies in heaven. But now the question is, would heavenly bodies fall under racial lines as we currently understand them in this life? The question is obviously unanswerable, but certain texts in the Bible after Jesus’ resurrection state that he did look different than he did while he was alive in earth.
Baker-Hytch (2021: 182) argues that “the new creation is depicted as an everlasting reality whose human inhabitants from all nations will have resurrection bodies that—after the pattern of Jesus’ resurrection body—neither age nor die and that will partake in shared pleasures such as eating and drinking together.” So there is a trend in Christian and theistic thought that in heaven, we will all have new heavenly bodies and not exist as mere disembodied souls. But talk of new heavenly bodies faces an issue—if they are bodies in the sense that we think of bodies now, the bodies that we inhabit now, then would they grow old, decay and eventually die? Would God then give us new heavenly bodies? It would stand to reason that, if God is indeed all-powerful and all-knowing, then he would have thought these issues through and so heavenly bodies wouldn’t have the same properties as physical, earthly bodies and so they wouldn’t get older, die and eventually decay.
Conclusion
If the afterlife is completely disembodied, then it follows that race wouldn’t exist in the afterlife, since there would be no way for the identities of persons to be established, and thusly there would be no way for the race of the disembodied soul to be established. Most theists contend that we will have new, heavenly bodies in heaven, but whether or not they would look the same as the former earthly bodies is up in the air, since Jesus after his resurrection apparently looked different, since it states in the Bible that it took some time for Jesus’ followers to recognize him. So, if Heaven exists, will there be races? The concept RACE is a physical one. So if there are disembodied souls in heaven, and they have no physical bodies, then races won’t exist in heaven.
I obviously am a realist about race who holds to radical pluralism about racial kinds—there can be many concepts of race which are true and are context-dependent. Though I do not believe in an afterlife, I do believe that if an afterlife is nothing but disembodied souls living in heaven wkth God, then it follows that there won’t be races in heaven since there are no physical bodies on which to ground racial ontologies. On the other hand, if what most theists contend is true—that we get new heavenly bodies after our death and entrance into the afterlife—whether or not race would exist in heaven is questionable and it depends on which concept of RACE one holds to. If one is a constructivist or skeptic (AKA eliminativist or anti-realist) about race, then race wouldn’t exist in heaven as race is due to social conventions and the concept of racialization of groups as races. But if one is a deflationary realist about race (which I myself am), then the answer to the question of whether or not races would exist in heaven is maybe.
Nevertheless, whether or not one believes in the existence of an afterlife is slightly drawn on racial lines, with blacks being more likely to believe in an afterlife compared to whites, while are more likely to believe that their prayers can be directly answered and that they can talk to a higher power in comparison to whites.
So depending on how races get squared away in heaven upon receiving new heavenly bodies, it is unknown whether or not races will exist in heaven.
Nutrition, Development, Epigenetics, and Physical Plasticity
1650 words
Humans are extremely “plastic”. “Plastic” meaning that our development can be shaped by what goes on (or does not go in) in our developmental environment along with the environment outside of the womb. Many factors drive development, and if one factor changes then part of the developmental course for the organism changes as well. Thus, environment can and does drive development, with the addition (or subtraction) of different factors. In this article, I will discuss some of the factors that drive development and physical plasticity and what can change them.
Subsistence provides food while food provides nutrition. Nutrients, then, supply our bodies with energy and promote tissue growth—among other things. However, nutrient requirements vary across and between species, while all mammals need a mixture of macronutrients (carbs, fat, protein, water, and fiber) and micronutrients (vitamins and minerals). Biological variability in nutrient requirements and “the eventual degree of metabolic function that an individual can achieve for a particular intake level is determined to a greater or lesser extent by genetic variants in enzymes controlling the absorption, uptake, distribution, retention or utilization of the nutrient” (Molloy, 2004: 156). Thus, individuals who consume the same amount of micro and macronutrients—who also have different polymorphisms in genes coding for the metabolism of any nutrient (through hormones and enzymes)—can, and do, have differing physiological responses to same vitamin intake. Thus, differences in genetic polymorphisms between individuals can—and do—lead to different disease.
Next we have phenotypic plasticity. Phenotypic plasticity, simply put, is the ability for a genome to express a different phenotype in variable environments. For instance, people born in hotter environments—no matter their race or ethnicity—develop larger pores in order to sweat more, since sweating is needed for cooling the body (Lieberman, 2015). Phenotypic plasticity can be a problem, though, in environments with numerous environmental stressors that will stress the mother and, in turn, affect the baby’s development in the womb as well affecting post-birth events. An example of this is when food availability is low and exposure to infection is high (in-utero and post-birth), and when these stressors are removed, the organism in question shows “catch-up growth”, implying that these stressors impeded the development of the organism in question.
Maternal nutritional imbalance has been found—both in animal studies and epidemiological studies—and metabolic disturbances, during critical windows of development for the organism, have both a persistent effect on the health of the organism and can be transmitted epigenetically to future generations (Gallou-Kabani and Junien, 2005). Gallou-Kabani and Junien (2005) write:
Epigenetic chromatin marks may be propagated mitotically and, in some cases, meiotically, resulting in the stable inheritance of regulatory states. Transient nutritional stimuli occurring at critical ontogenic stages may have lasting influences on the expression of various genes by interacting with epigenetic mechanisms and altering chromatin conformation and transcription factor accessibility (11).
Thus, metabolic syndrome can show transgenerational effects by way of incomplete erasure of the epigenetic factors carried by grandparents and parents. (See also Treretola et al, 2005.) Epigenetic regulation was extremely important during our evolution and especially during the development of the human organism, and is how and why we are so phenotypically plastic.
Epigenetic regulation during fetal reprogramming of the individual in preparation for the environment they expect to enter is likely to be a response to seasonal energy imbalance; changes that favour the metabolic efficiency are likely to be adaptive in such circumstances. Removal of seasonal energy stress, as has taken place in contemporary industrialized societies, may turn efficiency toward pathology. Humans thus have evolved an animal model that can respond genetically (through natural selection), phenotypically (through developmental plasticity) and epigenetically (by a balance of both). (Ulijaszek, Mann, and Elton, 2013: 19)
This seems to be a fundamental response to the human organism in-utero, responding to the lack of food in its environment and growing accordingly (low birth weight, susceptibilities to differing disease), which are still a problem for much of the developed world. Though this can be maladaptive in the developed, industrialized world, since poor early-life environments can lead to epigenetic changes which then spell out bad consequences for the low-birth-weight baby who was exposed to a slew of negative nutritional factors during conception (and post-birth).
It has already been established that nutrition can alter the genome and epigenome (Niculescu and Lupu, 2011; Niculescu, 2012; Anderson, Sant, and Dolinoy, 2012). So if differing nutritional effects can alter the genome and epigenome and these effects are transgenerationally inherited by future generations, then famines change the expression of the genome and epigenome which can then inherited by future generations if the epigenetic factors carried by the grandparents and parents are not erased (and there is mounting evidence for this claim, see Yang, Liu, and Sun, 2017).
There is evidence of phenotypic plasticity regarding the lack of nutrition when it comes to humans, in-utero, and the evidence comes from the Dutch Family Studies (see Lumey et al, 2007 for an overview of the project). Individuals who were prenatally exposed to the Dutch winter famine of 1944-45, six decades later, had less DNA methylation of the IGF2 (insulin-like growth factor 2) gene than same-sex siblings who were not exposed to the winter famine (Heijmns et al, 2008). The IGF2 gene plays an essential role of the development of the fetus before birth. The gene is highly active during fetal development, but much less so after birth. (It should be noted that the loss of imprinting on the IGF2 gene can promote prostate cancer; Fenner, 2017 and loss of imprinting on IGF2 can also promote other types of cancer as well; Livingstone, 2013).
Stein et al (2009) concluded that “famine exposure prior to conception is associated with poorer self-reported mental health and a higher level of depressive symptoms.” Tobi et al (2009) write that their data “support the hypothesis that associations between early developmental conditions and health outcomes later in life may be mediated by changes in the epigenetic information layer.” Tobi et al (2014) also show that the “Epigenetic modulation of pathways by prenatal malnutrition may promote an adverse metabolic phenotype in later life.” The prenatal—and neonatal—periods of development are of utmost importance in order for the organism to develop normally, any deviation outside of these measures can—and does—affect the genome and epigenome (Hajj et al, 2014).
Another strong example that these responses are adaptive to the organism in question is the fact that people who were exposed to nutritional imbalances in the womb showed a higher chance of becoming obese later in life (Roseboom, de Rooji, and Painter, 2006). Their study has implications for babies born in developing countries (since famines mirror, in a way, developing countries). Roseboom, de Rooji, and Painter (2006: 489) write:
This may imply that adaptations that enable the fetus to continue to grow may nevertheless have adverse consequences for health in later life.
Roseboom, de Rooji, and Painter (2006: 490) also write:
The nutritional experience of babies who were exposed to famine in early gestation may resemble that of babies in developing countries whose mothers are undernourished in early pregnancy and receive supplementation later on, but also of babies in developed countries whose mothers suffer from severe morning sickness.
So on-going studies, such as the Dutch Famine Study, have the chance to elucidate the mechanisms of low birth weight, and it can also show us how and why those exposed to adverse conditions in the womb show so many negative symptoms which are not present in kin who were not exposed to such malnutrition in the womb. These findings also suggest that nutrition before—and after—pregnancy can play a role in disease acquisition later in life. The fact that those exposed to famines have a higher chance of becoming obese later in life (Abeleen et al, 2012; Meng et al, 2017) shows that this adaptive response of the organism in the womb was very important in our evolution; the babe exposed to low maternal nutrition in the womb can, after birth, consume enough energy to become overweight, which would have been an adaptive evolutionary response to low maternal caloric energy.
Babies who are exposed to maternal under-nutrition in the womb—when exposed to an environment with ample foodstuffs—are at heightened risk of becoming type II diabetics and acquiring metabolic syndromes (Robinson, Buchholz, and Mazurak, 2007). This seems to be an adaptive, plastic response of the organism: since nutrients/energy were in low quantity in the womb, low nutrients/energy in the womb changed the epigenome of the organism, and so when (if) the organism is exposed to an environment with ample amounts of food energy, they will then have a higher susceptibility to metabolic syndromes and weight gains, due to their uterine environment. (Diet also has an effect on brain plasticity in both animals and humans, in the womb and out of it; see Murphy, Dias, and Thuret, 2014.)
In sum, phenotypic plasticity, which is driven in part by epigenetics, was extremely important in our evolution. This epigenetic regulation that occurs in the womb prepared the individual in question to be able to respond to the energy imbalance of the environment the organism was born in. The plasticity of humans, and animals, in regard to what occurs (or does not occur) in the environment, is how we were able to survive in new environments (not ancestral to our species). Epigenetic changes that occur in the grandparental and parental generations, when not completely erased during the meiotic division of cells, can affect future generations of progeny in a negative way.
The implications of the data are clear: under-nutrition (and malnutrition) affect the genome and epigenome in ways that are inherited through the generations, which is due to the physical plasticity of the human in-utero as well as post-birth when the baby developing. These epigenetic changes then lead to the one who experienced the adverse uterine environment to have a higher chance of becoming obese later in life, which suggests that this is an adaptive response to low amounts of nutrients/caloric energy in the uterine environment.
On Asian Body Fat and Diabetes
2000 words
Within-group differences in body fat and diabetes tell a lot about the diet and susceptibility of the diseases to that group. What the ethny does (or does not do) affects how high their body fat will be and whether or not they become diabetic. Since body fat levels are related to diabetes, then looking at both variables together should tell a lot about the diet and lifestyles of the ethnies studied. The ethnies I will look at are Chinese, Japanese, Filipinos, Koreans, Mongolians, and Filipinos.
Chinese
The Chinese have high levels of body fat (Wang et al, 2004) but have a lower BMI yet higher level of body fat than whites (Wang et al, 1994). BMI correlates with body fat percentage in the Chinese, while BMI and body fat percentage were related to DM (diabetes mellitus). Though BMI has its limits in people ranging from 24 to 27.9 BMI (Wang et al, 2011). New findings have shown that obesity in China may be underestimated (Gangqiang et al, 2017). That Chinese males have higher levels of body fat than white males held even after adjusting for age and BMI (Wang et al, 2011). The reality is that body fat percentage and diabetes, along with other diseases like prostate cancer (PCa) are increasing at an alarming rate in China (Tomlinson, Deng, and Thomas, 2008), so what is the cause?
The cause is very simple: The introduction of the Western diet. As I have written in the past, wherever the Western diet goes, diseases of civilization follow in high numbers in populations that previously did not eat that type of food. One analysis of the Chinese diet (compared with the Meditteranean, Japanese, and American diets) showed that “the Chinese diet has been shifting away from the traditional diet toward high-fat, low-carbohydrate and low-fiber diets, and nutrients intakes in Chinese people have been changing even worse than those in American people” (Zhang et al, 2015).
One study showed differences in dietary expectations between Americans (in Honolulu, Hawaii, so probably ethnically mixed) and Chinese in Changsha Hunan, China (Banna et al, 2016). The Chinese students mentioned physical outcomes such as “ such as maintaining immunity and digestive health” while American students state that they “balanced food groups” and balanced consumption with exercise (implying you can outrun a bad diet when you can’t…) while also stating that physical activity should be essential. American students stated that they needed to avoid foods high in fat. In that same manner, one Chinese student said “”Eat smaller amounts of meat, fish and vegetarian alternatives, choosing lower fat options whenever possible.” Meat, specifically beef and pork, was often cited as a food that should be limited” (Banna et al, 2016). Both groups of students in both countries erroneously assume that high-fat diets are bad for you—on the contrary, it’s high carb low-fat diets that are bad, which lead to DM.
The number of obese Chinese has surpassed the US; China is on its way to top the world in childhood obesity; and the incidence of diabetes is exploding in China. All due to the introduction of a Western diet. Something else worth noting: All Asian ethnies—at the same BMI—have higher levels of body fat and central adiposity, a risk-factor for diabetes (Deurenberg, Deurenberg-Yap, and Guricci, 2002).
Mongolians
Everywhere the Western Diet goes, obesity, diabetes, and disease soon follow and Mongolia is no different. Otgontuya et al (2009) showed that 6 percent of their study population were underweight, while 50.7 percent were in the normal range, 32.8 percent were overweight and 10.5 percent were obese, with women being slightly more likely to be overweight and obese. Rural people were more likely to be overweight and obese than urban people. Men had significantly lower body fat percent levels than women (26 and 34 percent respectively), women in the lowest age group had the lowest body fat percentage.
Mongolians living in China had impaired fasting glucose (IFG); those who had diabetes and IFG were more likely to be overweight and have higher central adiposity (Zhang et al, 2009). Mongolians eat an estimated 2,525 kcal per day, along with a fat/kcal ratio of 33.7—1.3 times higher than the Japanese and this is associated with their lower mortality (Komatsu et al, 2008).
Koreans
As with other Asian nations, Korea has the same problems. Hong et al (2011) showed that in Korean men, muscle mass decreases and body fat increases with age while for women fat mass and obesity increased with age. I particularly like this study since they assessed percent body fat (and other variables) with the DXA scan—one of the gold-standard of assessing body fat. Another Korean study showed that high birthweight leads to obesity and higher levels of body fat but not muscle mass (Kang et al, 2018), and with the advent of the Western diet in Asia, we can expect higher rates of obesity. (Note that this is an observational study and thusly causation is not certain, future studies will tease out causation and I bet the Western diet plays a role.) Another study even showed that eating frequency is related to obesity when diet quality is high, but not low in Korean adults (Kim, Yang, and Park, 2018).
There is one more risk-factor in regard to Korean obesity—study time after school is associated with habitual eating which leads to becoming overweight and obese. In this sample, Korean children who reported studying after school and eating when they were not hungry during studying were at increased risk for developing obesity in later years (Lee et al, 2018).
There is one interesting thing to note in regard to Koreans and diabetes, though: High leg fat mass, along with lower leg muscle mass, significantly lowered the risk for DM, while those who had lower leg body fat but higher leg muscle mass had a higher risk for developing diabetes (Choi et al, 2017). Shin, Hong, and Shin (2017) show that “… BAI is less useful than BMI and other adiposity indices, such as the WHtR, the WHR, and WC. These indices may be better candidates for clinical use and to evaluate metabolic syndrome risk factors.” One mouse study showed that the traditional Korean diet prevented obesity and ameliorated insulin resistance (Choi et al, 2017) which implies that a shift back to the traditional Korean diet for Koreans would show positive health benefits.
Japanese
Japan is similar to China as regards body fat percentage and BMI. They have a culture of fat-shaming (do note that it does not work but in fact makes the problem worse due to biochemical stress) and when one of their peers becomes overweight, they begin to shame in hopes that they will lower their weight. Though, despite their culture of thinness, in Japan, diabetes is a “hidden scourge“. This is due to, again, the Western diet reaching Japanese shores.
Rice is a major food staple in Japan. Since rice is a carbohydrate, then it follows that, if eaten in large amounts, one who eats more rice than another would have a higher chance of becoming a diabetic. Rice intake is associated with the onset of diabetes in Japanese women, with a significant increase in diabetes if the woman ate more than 420 grams of rice (3 bowls) per day; the association was pronounced in women who were physically-inactive, and nonobese (Nanri et al, 2010). The same was seen in Chinese women (Villegas et al, 2007).
However, Nanri et al (2010) state that “The mechanism by which increased rice consumption increases risk of type 2 diabetes remains unclear. … the association between rice intake and type 2 diabetes risk remained significant even after adjustment for these food factors, which suggested an independent role of white rice in the pathogenesis of type 2 diabetes.” The cause is very simple: White rice, as Nanri et al note, is high on the glycemic index scale. If a food is high on the glycemic index scale, then it will spike one’s blood sugar high, which eventually would lead to DM. It’s also worth noting that a low-carb diet was associated with a decrease in diabetes, most likely due to a decrease in white rice consumption (Nanri et al, 2015).
The Japanese, in comparison to other Asian countries, have low levels of obesity, though the maladies they acquire are in-line with their diet and what they eat. However, some have noted the fact that Japanese diabetes rates are low. (Notwithstanding their hidden scourge.) This is easily explainable: The percent of carbohydrate intake is nowhere as important as the absolute amount of carbohydrate consumed. Though their diabetic population has increased to over 10 million recently. This is, of course, due to the introduction of the Western diet in Japan.
Filipinos
The last ethny I will discuss are Filipinos. Body-shaming is, as it is in other Asian countries, prevalent. At a fixed BMI, in spite of both groups living in similar conditions and eating a similar diet, “Malay and Thai boys had a significantly higher %BF than Filipino boys and Thai girls had a significantly higher %BF than Malay and Filipino girls” (Liu et al, 2011).
Choi et al (2013) showed that Filipino men living in California with DM were more likely to be overweight and obese, and Filipino men without DM were still more likely to be overweight and obese (even when adjusting for age and other lifestyle factors, Filipinos still had a higher chance of acquiring DM. Though Korean women had the highest rates of DM, followed by Filipinas.
Filipino and Korean emigrants to America had higher rates of weight gain than Chinese emigrants (Oakkert et al, 2015). This could be due to cultural values back home, which then obviously change when they emigrate to America. Furthermore, they find themselves in obesogenic environments (See Lake and Townshend,2006; Townshend and Lake, 2017). The cause is the difference in the built food environment; this is why Filipino men and women have high rates of DM and CVD (cardiovascular disease).
Further, in Filipinas, increased socioeconomic status, urban residence, fewer pregnancies and lactations and spending more time away from home is positively associated with weight gain. Though a high waist-to-hip ratio and being overweight and obese was independently related to hypertension in Filipinas (Adair, 2012). This study documented weight changes in a 16-year period in Filipina women as they moved higher up the SES ladder. Adair (2012) does note that obesity is increasing in lower-income households, too, but not as quickly when compared to more affluent households.
Comparing body fat percentages amongst Asian-American groups indicates that not all Asian-American populations are not equal in body fatness (Alpert and Thomason, 2016). However, one study shows that Asian Indians and Filipinos had higher prevalences of being overweight (35-37 percent and 35-47 percent respectively; Oza-Frank et al, 2009). This analysis, along with many others, shows that Asians—no matter the ethny—have higher levels of body fat than non-Hispanic white populations. It’s also worth noting that Filipina women had higher levels of VAT (visceral adipose tissue) than whites of a similar BMI and WC (waist circumference; Araneta and Barrett-Connor, 2012).
Conclusion
Asian ethnies have differing levels of body fat at the same BMI. This implies that what works for whites regarding BMI won’t work for Asians, since these ethnies, when compares with whites of a similar BMI and WC, had higher rates of body fat. The relationship between BMI and body fat levels is ethny-specific (Deurenberg, Deurenberg-Yap, and Guricci, 2002), though Filipinos and Asian Indians have higher levels of body fat regardless of the BMI standard used (Oza-Frank et al, 2009), which is one of the most important tells in ascertaining whether one is at-risk for DM and other maladies. It is not particularly interesting that Asian emigrants to America see their weight increase, as this is noted when the scourge called the Western diet crosses the Pacific. But what is interesting here is the rates between each Asian ethny, what they eat, and what causes the relationship.
Asian ethnies, when matched at similar BMIs, had differing levels of body fat, which implies that there should be ethny-specific BMI, though no matter which BMI standard was used, Filipinos and Asian Indians still had higher rates of body fat.
Calories are not Calories
1300 words
More bullocks from Dr. Thompson:
I say that if you are over-weight and wish to lose weight, then you should eat less. You should keep eating less until you achieve your desired weight, and then stick to that level of calorific intake.
Why only talk about calories and assume that they do the same things once ingested into the body? See Feinman and Fine (2004) to see how and why that is fallacious. This was actually studied. Contestants on the show The Biggest Loser were followed after they lost a considerable amount of weight. They followed the same old mantra: eat less, and move more. Because if you decrease what is coming in, and expend more energy then you will lose weight. Thermodynamics, energy in and out, right? That should put one into a negative energy balance and they should lose weight if they persist with the diet. And they did. However, what is going on with the metabolism of the people who lost all of this weight, and is this effect more noticeable for people who lost more weight in comparison to others?
Fothergill et al (2016) found that persistent metabolic slowdown occurred after weight loss, the average being a 600 kcal slowdown. This is what the conventional dieting advice gets you, a slowed metabolism with you having to eat fewer kcal than one who was never obese. This is what the ‘eat less, move more’ advice, the ‘CI/CO’ advice is horribly flawed and does not work!
He seems to understand that exercise does not work to induce weight loss, but it’s this supposed combo that’s supposed to be effective, a kind of one-two punch, and you only need to eat less and move more if you want to lose weight! This is horribly flawed. He then shows a few table from a paper he authored with another researcher back in 1974 (Bhanji and Thompson, 1974).
Say you take 30 people who weigh the same, have the same amount of body fat and are the same height, they eat the same exact macronutrient composition, with the same exact foods, eating at a surplus deficit with the same caloric content, and, at the end of say, 3 months, you will get a different array of weight gained/stalled/decrease in weight. Wow. Something like this would certainly disprove the CI/CO myth. Aamodt (2016: 138-139) describes a study by Bouchard and Tremblay (1997; warning: twin study), writing:
When identical twins, men in their early 20s, were fed a thousand extra calories per day for about three months, each pair showed similar weight gains. In contrast, the gains varied across twin pairs, ranging from nine to twenty-nine pound, even though the calorie imbalance esd the same for everyone. An individual’s genes also influence weight loss. When another group of identical twins burned a thousand more calories per day through exercise while maintaining a stable food intake in an inpatient facility, their losses ranged from two to eighteen pounds and were even more similar within twin pairs than weight gain.
Take a moment to think about that. Some people’s bodies resis weight loss so well that burning an extra thousand calpires a day for three months, without eating more, leads them to lose only two pounds. The “weight loss is just math” crows we met in the last chapter needs to look at what happens when their math is applied to living people. (We know what usually happens: they accuse the poor dieter of cheating, whether or not it’s true.) If cutting 3,500 calories equals one pound of weight loss, then everyone on the twuns’ exercist protocol should have lost twenty-four pounds, but not a single participant lost that much. The average weight loss was only eleven pounds, and the individual variation was huge. Such differences can result from genetic influences on resting metabolism, which varies 10 to 15 percent between people, or from differences in the gut. Because the thousand-calorie energy imbalance was the same in both the gain and loss experiments, this twin research also illustrates that it’s easier to gain weight than to lose it.
That’s weird. If a calorie were truly a calorie, then, at least in the was CI/COers word things, everyone should have had the same or similar weight loss, not with the average weight loss less than half what should have been expected from the kcal they consumed. That is a shot against the CI/CO theory. Yet more evidence against comes from the Vermont Prison Experiment (see Salans et al, 1971). In this experiment, they were given up to 10,000 kcal per day and they, like in the other study described previously, all gained differing amounts of weight. Wow, almost as if individuals are different and the simplistic caloric math of the CI/COers doesn’t size up against real-life situations.
The First Law of Thermodynamics always holds, it’s just irrelevant to human physiology. (Watch Gary Taubes take down this mythconception too; not a typo.) Think about an individual who decreases total caloric intake from 1500 kcal per day to 1200 kcal per day over a certain period of time. The body is then forced to drop its metabolism to match the caloric intake, so the metabolic system of the human body knows when to decrease when it senses it’s getting less intake, and for this reason the First Law is not violated here, it’s irrelevant. The same thing also occurred to the Biggest Loser contestants. Because the followed the CI/CO paradigm of ‘eat less and move more’.
Processed food is not bad in itself, but it is hard to monitor what is in it, and it is probably best avoided if you wish to lose weight, that is, it should not be a large part of your habitual intake.
If you’re trying to lose weight you should most definitely avoid processed foods and carbohydrates.
In general, all foods are good for you, in moderation. There are circumstances when you may have to eat what is available, even if it is not the best basis for a permanent sustained diet.
I only contest the ‘all foods are good for you’ part. Moderation, yes. But in our hedonistic world we live in today with a constant bombardment of advertisements there is no such thing as ‘moderation’. Finally, again, willpower is irrelevant to obesity.
I’d like to know the individual weight gains in Thompson’s study. I bet it’d follow both what occurred in the study described by Aamodt and the study by Sims et al. The point is, human physiological systems are more complicated than to attempt to break down weight loss to only the number of calories you eat, when not thinking of what and how you eat it. What is lost in all of this is WHEN is a good time to eat? People continuously speak about what to eat, where to eat, how to eat, who to eat with but no one ever seriously discusses WHEN to eat. What I mean by this is that people are constantly stuffing their faces all day, constantly spiking their insulin which then causes obesity.
The fatal blow for the CI/CO theory is that people do not gain or lose weight at the same rate (I’d add matched for height, overall weight, muscle mass and body fat, too) as seen above in the papers cited. Why people still think that the human body and its physiology is so simple is beyond me.
Hedonism along with an overconsumption of calories consumed (from processed carbohydrates) is why we’re so fat right now in the third world and the only way to reverse the trend is to tell the truth about human weight loss and how and why we get fat. CI/CO clearly does not work and is based on false premises, no matter how much people attempt to save it. It’s highly flawed and assumed that the human body is so ‘simple’ as to not ‘care’ about the quality of the macro nor where it came from.
Is Diet An IQ Test?
1350 words
Dr. James Thompson is a big proponent of ‘diet being an IQ test‘ and has written quite a few articles on this matter. Though, the one he published today is perhaps the most misinformed.
He first shortly discusses the fact that 200 kcal drinks are being marketed as ‘cures’ for type II diabetes. People ‘beat’ the disease with only 200 kcal drinks. Sure, they lost weight, lost their disease. Now what? Continue drinking the drinks or now go back to old dietary habits? Type II diabetes is a lifestyle disease, and so can be ameliorated with lifestyle interventions. Though, Big Pharma wants you to believe that you can only overcome the disease with their medicines and ‘treatments’ along with the injection of insulin from your primary care doctor. Though, this would only exacerbate the disease, not cure it. The fact of the matter is this: these ‘treatments’ only ‘cure’ the proximate causes. The ULTIMATE CAUSES are left alone and this is why people fall back into habits.
When speaking about diabetes and obesity, this is a very important distinction to make. Most doctors, when treating diabetics, only treat the proximate causes (weight, symptoms that come with weight, etc) but they never get to the root of the problem. The root of the problem is, of course, insulin. The main root is never taken care of, only the proximate causes are ‘cured’ through interventions, however, the underlying cause of diabetes, and obesity as well is not taken care of because of doctors. This, then, leads to a neverending cycle of people losing a few pounds or whatnot and then they, expectedly, gain it back and they have to re-do the regimen all over again. The patient never gets cured, Big Pharma, hospitals et al get to make money off not curing a patients illness by only treating proximate and not ultimate causes.
Dr. Thompson then talks about a drink for anorexics, called ‘Complan“, and that he and another researcher gave this drink to anorexics, giving them about 3000 kcals per day of the drink, which was full of carbs, fat and vitamins and minerals (Bhanji and Thompson, 1974).
The total daily calorific intake was 2000-3000 calories, resulting in a mean weight gain of 12.39 kilos over 53 days, a daily gain of 234 grams, or 1.64 kilos (3.6 pounds) a week. That is in fact a reasonable estimate of the weight gains made by a totally sedentary person who eats a 3000 calorie diet. For a higher amount of calories, adjust upwards. Thermodynamics.
Thermodynamics? Take the first law. The first law of thermodynamics is irrelevant to human physiology (Taubes, 2007; Taubes, 2011; Fung, 2016). (Also watch Gary Taubes explain the laws of thermodynamics.) Now take the second law of thermodynamics which “states that the total entropy can never decrease over time for an isolated system, that is, a system in which neither energy nor matter can enter nor leave.” People may say that ‘a calorie is a calorie’ therefore it doesn’t matter whether all of your calories come from, say, sugar or a balanced high fat low carb diet, all weight gain or loss will be the same. Here’s the thing about that: it is fallacious. Stating that ‘a calorie is a calorie’ violates the second law of thermodynamics (Feinman and Fine, 2004). They write:
The second law of thermodynamics says that variation of efficiency for different metabolic pathways is to be expected. Thus, ironically the dictum that a “calorie is a calorie” violates the second law of thermodynamics, as a matter of principle.
So talk of thermodynamics when talking about the human physiological system does not make sense.
He then cites a new paper from Lean et al (2017) on weight management and type II diabetes. The authors write that “Type 2 diabetes is a chronic disorder that requires lifelong treatment. We aimed to assess whether intensive weight management within routine primary care would achieve remission of type 2 diabetes.” To which Dr. Thompson asks ‘How does one catch this illness?” and ‘Is there some vaccination against this “chronic disorder”?‘ The answer to how does one ‘catch this illness’ is simple: the overconsumption of processed carbohydrates, constantly spiking insulin which leads to insulin resistance which then leads to the production of more insulin since the body is resistant which then causes a vicious cycle and eventually insulin resistance occurs along with type II diabetes.
Dr. Thompson writes:
Patients had been put on Complan, or its equivalent, to break them from the bad habits of their habitual fattening diet. This is good news, and I am in favour of it. What irritates me is the evasion contained in this story, in that it does not mention that the “illness” of type 2 diabetes is merely a consequence of eating too much and becoming fat. What should the headline have been?
Trial shows that fat people who eat less become slimmer and healthier.
I hope this wonder treatment receives lots of publicity. If you wish to avoid hurting anyone’s feelings just don’t mention fatness. In extremis, you may talk about body fat around vital organs, but keep it brief, and generally evasive.
So you ‘break bad habits’ by introducing new bad habits? It’s not sustainable to drink these low kcal drinks and expect to be healthy. I hope this ‘wonder treatment’ does not receive a lot of publicity because it’s bullshit that will just line the pockets of Big Pharma et al, while making people sicker and, the ultimate goal, having them ‘need’ Big Pharma to care for their illness—when they can just as easily care for it themselves.
‘Trial shows that fat people who eat less become slimmer and healthier’. Or how about this? Fat people that eat well and exercise, up to 35 BMI, have no higher risk of early death then someone with a normal BMI who eats well and exercises (Barry et al, 2014). Neuroscientist Dr. Sandra Aamodt also compiles a wealth of solid information on this subject in her 2016 book “Why Diets Make Us Fat: The Unintended Consequences of Our Obsession with Weight Loss“.
Dr. Thompson writes:
I see little need to update the broad conclusion: if you want to lose weight you should eat less.
This is horrible advice. Most diets fail, and they fail because the ‘cures’ (eat less, move more; Caloric Reduction as Primary: CRaP) are garbage and don’t take human physiology into account. If you want to lose weight and put your diabetes into remission, then you must eat a low-carb (low carb or ketogenic, doesn’t matter) diet (Westman et al, 2008; Azar, Beydoun, and Albadri, 2016; Noakes and Windt, 2016; Saslow et al, 2017). Combine this with an intermittent fasting plan as pushed by Dr. Jason Fung, and you have a recipe to beat diabesity (diabetes and obesity) that does not involve lining the pockets of Big Pharma, nor does it involve one sacrificing their health for ‘quick-fix’ diet plans that never work.
In sum, diets are not ‘IQ tests’. Low kcal ‘drinks’ to ‘change habits’ of type II diabetics will eventually exacerbate the problem because when the body is in extended caloric restriction, the brain panics and releases hormones to stimulate appetite while stopping hormones that cause you to be sated and stop eating. This is reality; these studies that show that eating or drinking 800 kcal per day or whatnot are based on huge flaws: the fact that this could be sustainable for a large number of the population is not true. In fact, no matter how much ‘willpower’ you have, you will eventually give in because willpower is a finite resource (Mann, 2014).
There are easier ways to lose weight and combat diabetes, and it doesn’t involve handing money over to Big Pharma/Big Food. You only need to intermittently fast, you’ll lose weight and your diabetes will not be a problem, you’ll be able to lose weight and will not have problems with diabetes any longer (Fung, 2016). Most of these papers coming out recently on this disease are garbage. Real interventions exist, they’re easier and you don’t need to line the pockets of corporations to ‘get cured’ (which never happens, they don’t want to cure you!)
Black-White Differences in Physiology
2050 words
Black-white differences in physiology can tell a lot about how the two groups have evolved over time. On traits like resting metabolic rate (RMR), basal metabolic rate (BMR), adiposity, heart rate, Vo2 max, etc. These differences in physiological variables between groups, then, explain part of the reason why there are different outcomes in terms of life quality/mortality between the two groups.
Right away, by looking at the average black and average white, you can see that there are differences in somatype. So if there are differences in somatype, then there must be differences in physiological variables, and so, this may be a part of the cause of, say, differing obesity rates between black and white women (Albu et al, 1997) and even PCOS (Wang and Alvero, 2013).
Resting metabolic rate
Resting metabolic rate is your body’s metabolism at rest, and is the largest component of the daily energy budget in modern human societies (Speakman and Selman, 2003). So if two groups, on average, differ in RMR, then one with the lower RMR may have a higher risk of obesity than the group with the higher RMR. And this is what we see.
Black women do, without a shadow of a doubt, have a lower BMR, lower PAEE (physical activity energy expenditure) and TDEE (total daily expenditure) (Gannon, DiPietro, and Poehlman, 2000). Knowing this, then it is not surprising to learn that black women are also the most obese demographic in the United States. This could partly explain why black women have such a hard time losing weight. Metabolic differences between ethnic groups in America—despite living in similar environments—show that a genetic component is responsible for this.
There are even predictors of obesity in post-menopausal black and white women (Nicklas et al, 1999). They controlled for age, body weight and body composition (variables that would influence the results—no one tell me that “They shouldn’t have controlled for those because it’s a racial confound!”) and found that despite having a similar waist-to-hip ratio (WHR) and subcutaneous fat area, black women had lower visceral fat than white women, while fasting glucose, insulin levels, and resting blood pressure did not differ between the groups. White women also had a higher Vo2 max, which remained when lean mass was controlled for. White women could also oxidize fat at a higher rate than black women (15.4 g/day, which is 17% higher than black women). When this is expressed as percent of total kcal burned in a resting state, white women burned more fat than black women (50% vs 43%). I will cover the cause for this later in the article (one physiologic variable is a large cause of these differences).
We even see this in black American men with more African ancestry—they’re less likely to be obese (Klimentidis et al 2016). This, too, goes back to metabolic rate. Black American men have lower levels of body fat than white men (Vickery et al, 1988; Wagner and Heyward, 2000). All in all, there are specific genetic variants and physiologic effects, which cause West African men to have lower central (abdominal) adiposity than European men and black women who live in the same environment as black men—implying that genetic and physiologic differences between the sexes are the cause for this disparity. Whatever the case may be, it’s interesting and more studies need to be taken out so we can see how whatever gene variants are *identified* as protecting against central adiposity work in concert with the system to produce the protective effect. Black American men have lower body fat, therefore they would have, in theory, a higher metabolic rate and be less likely to be obese—while black women have the reverse compared to white women—a lower metabolic rate.
Skeletal muscle fiber
Skeletal muscle fibers are the how and why of black domination in explosive sports. This is something I’ve covered in depth. Type II fibers contract faster than type I. This has important implications for certain diseases that black men are more susceptible to. Though the continuous contraction of the fibers during physical activity leads to a higher disease susceptibility in black men—but not white men (Tanner et al, 2001). If you’re aware of fiber type differences between the races (Ama et al, 1986; Entine, 2000; Caeser and Henry, 2015); though see Kerr (2010’s) article The Myth of Racial Superiority in Sports for another view. That will be covered here in the future.
Nevertheless, fiber typing explains racial differences in sports, with somatype being another important variable in explaining racial disparities in sports. Two main variables that work in concert are the somatype (pretty much body measurements, length) and the fiber type. This explains why blacks dominate baseball and football; this explains why ‘white men can’t jump and black men can’t swim’. Physiological variables—not only ‘motivation’ or whatever else people who deny these innate differences say—largely explain why there are huge disparities in these sports. Physiology is important to our understanding of how and why certain groups dominate certain sports.
This is further compounded by differing African ethnies excelling in different running sports depending on where their ancestors evolved. Kenyans have an abundance of type I fibers whereas West Africans have an abundance of type II fibers. (Genetically speaking, ‘Jamaicans’ don’t exist; genetic testing shows them to come from a few different West African countries.) Lower body symmetry—knees and ankles—show that they’re more symmetrical than age-matched controls (Trivers et al, 2014). This also goes to show that you can’t teach speed (Lombardo and Deander, 2014). Though, of course, training and the will to want to do your best matter as well—you just cannot excel in these competitions without first and foremost having the right physiologic and genetic make-up.
Further, although it’s only one gene variant, ACTN3 and ACE explain a substantial percentage of sprint time variance, which could be the difference between breaking a world record and making a final (Papadimitriou et al, 2016). So, clearly, certain genetic variants matter more than others—and the two best studied are ACTN3 and ACE. Some authors, though, may deny the contribution of ACTN3 to elite athletic performance—like one researcher who has written numerous papers on ACTN3, Daniel MacArthur. However, elite sprinters are more likely to carry the RR ACTN3 genotype compared to the XX ACTN3 genotype, and the RR ACTN3 genotype—when combined with type II fibers and morphology—lead to increased athletic performance (Broos et al, 2016). It’s also worth noting that 2 percent of Jamaicans carry the XX ACTN3 genotype (Scott et al, 2010), so this is another well-studied variable that lends to superior running performance in Jamaicans.
In regards to Kenyans, of course when you are talking about genetic reasons for performance, some people don’t like it. Some may say that certain countries dominate in X, and that for instance, North Africa is starting to churn out elite athletes, should we begin looking for genetic advantages that they possess (Hamilton, 2000)? Though people like Hamilton are a minority view in this field, I have read a few papers that there is no evidence that Kenyans possess a pulmonary system that infers a physiologic advantage over whites (Larsen and Sheel, 2015).
People like these three authors, however, are in the minority here and there is a robust amount of research that attests to East African running dominance being genetic/physiologic in nature—though you can’t discredit SES and other motivating variables (Tucker, Onywera, and Santos-Concejero, 2015). Of course, a complex interaction between SES, genes, and environment are the cause of the success of the Kalenjin people of Kenya, because they live and train in such high altitudes (Larsen, 2003), though the venerable Bengt Saltin states that the higher Vo2 max in Kenyan boys is due to higher physical activity during childhood (Saltin et al, 1995).
Blood pressure
The last variable I will focus on (I will cover more in the future) is blood pressure. It’s well known that blacks have higher blood pressure than whites—with black women having a higher BP than all groups—which then leads to other health implications. Some reasons for the cause are high sodium intake in blacks (Jones and Hall, 2006); salt (Lackland, 2014; blacks had a similar sensitivity than whites, but had a higher blood pressure increase); while race and ethnicity was a single independent predictor of hypertension (Holmes et al, 2013). Put simply, when it comes to BP, ethnicity matters (Lane and Lip, 2001).
While genetic factors are important in showing how and why certain ethnies have higher BP than others, social factors are arguably more important (Williams, 1992). He cites stress, socioecologic stress, social support, coping patterns, health behavior, sodium, calcium, and potassium consumption, alcohol consumption, and obesity. SES factors, of course, lead to higher rates of obesity (Sobal and Stunkard, 1989; Franklin et al, 2015). So, of course, environmental/social factors have an effect on BP—no matter if the discrimination or whatnot is imagined by the one who is supposedly discriminated against, this still causes physiologic changes in the body which then lead to higher rates of BP in certain populations.
Poverty does affect a whole slew of variables, but what I’m worried about here is its effect on blood pressure. People who are in poverty can only afford certain foods, which would then cause certain physiologic variables to increase, exacerbating the problem (Gupta, de Wit, and McKeown, 2007). Whereas diets high in protein predicted lower BP in adults (Beundia et al, 2015). So this is good evidence that the diets of blacks in America do increase BP, since they eat high amounts of salt, low protein and high carb diets.
Still, others argue that differences in BP between blacks and whites may not be explained by ancestry, but by differences in education, rather than genetic factors (Non, Gravlee, and Mulligan, 2012). Their study suggests that educating black Americans on the dangers and preventative measures of high BP will reduce BP disparities between the races. This is in-line with Williams (1992) in that the social environment is the cause for the higher rates of BP. One hypothesis explored to explain why this effect with education was greater in blacks than whites was that BP-related factors, such as stress, poverty and racial discrimination (remember, even if no racial discrimination occurs, any so-called discrimination is in the eye of the beholder so that will contribute to a rise in physiologic variables) and maybe social isolation may be causes for this phenomenon. Future studies also must show how higher education causes lower BP, or if it only serves as other markers for the social environment. Nevertheless, this is an important study in our understanding of how and why the races differ in BP and it will go far to increase our understanding of this malady.
Conclusion
This is not an exhaustive list—I could continue writing about other variables—but these three are some of the most important as they are a cause for higher mortality rates in America. Understanding the hows and whys of these variables will have us better equipped to help those who suffer from diseases brought on by these differences in physiological factors.
The cause for some of these physiologic differences come down to evolution, but still others may come down to the immediate obesogenic environment (Lake and Townshend, 2006) which is compounded by lower SES. Since high carbs diets increase BP, this explains part of the reason why blacks have higher BP, along with social and genetic factors. Muscle fiber typing is set by the second trimester, and no change is seen after age 6 (Bell, 1980). Resting metabolic rate gap differences between black and white women can be closed, but not completely, if black women were to engage in exercise that use their higher amounts of type II muscle fibers (Tanner et al, 2001). This research is important to understand differences in racial mortality; because when we understand them then we can begin to theorize on how and why we see these disparities.
Physiologic differences between the races are interesting, they’re easily measurable and they explain both disparities in sports and mortality by different diseases. Once we study these variables more, we will be better able to help people with these variables—race be dammed. Race is a predictor here, only because race is correlated with other variables that lead to negative health outcomes. So once we understand how and why these differences occur, then we can help others with similar problems—no matter their race.
Weight Loss and the Microbiome
1450 words
Last month I argued that there was more to weight loss than CI/CO. One of the culprits is a virus called Ad-36. Obese people are more likely to have Ad-36 antibodies in comparison to lean people, which implies that they have/had the virus and could be a part of the underlying cause of obesity. However, a paper was recently published that your stool can predict whether or not you can lose weight. This is due to how certain bacteria in the gut respond to different macronutrients ingested into the body.
ScienceDaily published an article a few days ago titled Your stools reveal whether you can lose weight. In the article, they describe the diets of the cohort, which followed 31 people, some followed the New Nordic Diet (NND), while others followed the Average Danish Diet (ADD) (Hjorth et al, 2017; I can’t find this study!! I’ll definitely edit this article after I read the full paper when it is available). So 31 people ate the NDD for 26 weeks, and lost 3.5 kg (7.72 pounds for those of us who use freedom numbers) while those who ate the ADD lost an average of 1.7 kg (3.75 pounds for those of us who use freedom numbers). So there was a 1.8 kg difference in pounds lost between the two diets. Why?
Here’s the thing: when people were divided by their microbiota, those who had a higher proportion of Prevotella to Bacteriodoites lost 3.5 more kg (7.72 pounds) in 26 weeks when they ate the NND in comparison to the ADD. Those who had a lower proportion of Prevotella to Bacteriodoites lost no additional weight on the NND. Overall, they say, about 50 percent of the population would benefit from the NND, while the rest of the population should diet and exercise until new measures are found.
The New Danish Diet is composed of grains, fruits, and vegetables. The diet worked for one-half of the population, but not for the other. The researchers state that people should try other diets and to exercise for weight loss while they study other measures. This is important to note: the same diet did not induce weight loss in a population; the culprit here is the individual microbiome.
Now that those Bacteroidotes have come up again, this quote from Allana Collen’s 2014 book 10% Human: How Your Body’s Microbes Hold the Key to Health and Happiness:
But before we get too excited about the potential for a cure for obesity, we need to know how it all works. What are these microbes doing that make us fat? Just as before, the microbiotas in Turnbaugh’s obese mice contained more Firmicutes and fewer Bacteroidetes, and they somehow seemed to enable the mice to extract more energy from their food. This detail undermines one of the core tenets of the obesity equation. Counting ‘calories-in’ is not as simple as keeping track of what a person eats. More accurately, it is the energy content of what a person absorbs. Turnbaugh calculated that the mice with the obese microbiota were collecting 2 per cent more calories from their food. For every 100 calories the lean mice extracted, the obese mice squeezed out 102.
Not much, perhaps, but over the course of a year or more, it adds up. Let’s take a woman of average height. 5 foot 4 inches, who weights 62 kg (9st 11 lb) and a healthy Body Mass Index (BMI: weight (kg) /(height (m)^2) of 23.5. She consumes 2000 calories per day, but with an ‘obese’ microbiota, her extra 2 per cent calorie extraction adds 40 more calories each day. Without expending extra energy, those further 40 calories per day should translate, in theory at least, to a 1.9 kg weight gain over a year. In ten years, that’s 19 kg, taking her weight to 81 kg (12 st 11 lb) and her BMI to an obese 30.7. All because of just 2 percent extra calories extracted from her food by her gut bacteria.
This corresponds with the NND/ADD study on weight loss… This proves that there is more than the simplistic CI/CO to weight loss, and that an individual’s microbiome/physiology definitely does matter in regards to weight loss. Clearly, to understand the population-wide problem of obesity we must understand the intricate relationship between the microbiome/brain/gut/body relationship and how it interacts with what we eat. Because evidence is mounting that the individual’s microbiome houses the key to weight loss/gain.
Exercise does not induce weight loss. A brand new RCT (randomized controlled trial) showed that in a cohort of children who were made to do HIIT (high-intensity interval training) did show better cardiorespiratory fitness, but there were no concomitant reductions in adiposity and bio blood markers (Dias et al, 2017). What this tells me is that people should exercise for health and that ‘high’ that comes along with it; if people exercise for weight loss they will be highly disappointed. Note, I am NOT saying to not exericse, I’m only saying to not have any unrealistic expectations that cardio will induce it, it won’t!
Bjornara et al (2016) showed that, when the NND was compared to the ADD, there was better adherence to the NND when compared to the ADD. Poulskin et al (2015) showed that the NND provided higher satisfaction, and body weight reduction with higher compliance with the NND and with physical activity (I disagree there, see above).
This study is important for our understanding of weight loss for the population as a whole. More recent evidence has shown that our microbiome and body clock work together to ‘pack on the pounds‘. This recent study found that the microbiome “regulate[s] lipid (fat) uptake and storage by hacking into and changing the function of the circadian clocks in the cells that line the gut.” The individual microbiome could induce weight gain, especially when they consume a Western diet, which of course is full of fat and sugar. One of the most important things they noticed is that mice without a microbiome fared much better on a high-fat diet.
The microbiome ‘talks’ to the gut lining. Germ-free mice were genetically unable to make NFIL3 in the cell lining of the gut. So germ-free mice lack a microbiome and lower than average production of NFIL3, meaning they take up and store fewer lipids than those with a microbiome.
So the main point about this study is the circadian rhythm. The body’s circadian clock recognizes the day/night system, which of course are linked to feeding times, which turn the body’s metabolism on and off. Cells are not directly exposed to light, but they capture light cues from visual and nervous systems, which then regulates gene expression. The gut’s circadian clock then regulates the expression of NFIL3 and the lipid metabolic machinery which is controlled NFIL3. So this study shows how the microbiome interacts with and impacts metabolism. This could also, as the authors state, explain how and why people who work nights and have shift-work disorder and the concurrent metabolic syndromes that come along with it.
In regards to the microbiome and weight loss, it is poorly understood at the moment (Conlon and Bird, 2015), though a recent systematic review showed that restrictive diets and bariatric surgery “reduce microbial abundance and promote changes in microbial composition that could have long-term detrimental effects on the colon.” They further state that “prebiotics might restore a healthy microbiome and reduce body fat“(Segenfrado et al, 2017). Wolf and Lorenz (2012) show that using “good” probiotic bacteria may induce changes in the obese phenotype. Bik (2015) states that learning more about the microbiome, dysbiosis (Carding et al, 2015), and how the microbiome interacts with our metabolism, brain, and physiology, then we can better treat those with obesity due to the dysbiosis of the microbiome. Clark et al (2012) show how the mechanisms behind the microbiota and obesity.
Weight loss is, clearly, more than CI/CO, and once we understand other mechanisms of weight loss/gain/regulation then we can better treat people with these metabolic syndromes that weirdly are all linked to each other. Diets affect the diversity of the microbiome, the diversity of the microbiome already there though, may need other macro/micro splits in order to show differing weight loss, in the case of the NND and ADD study reviewed above. Changes in weight do change the diversity of the microbiome of an individual, however, the heritable component of the microbiome may mean that some people need to eat different foods compared to others who have a different microbiome. Over time, new studies will show how and why the macro/micronutrient content matters for weight loss/gain.
Clearly, reducing the complex physiological process of weight gain/loss to numbers and ignoring the physiological process and how the microbiome induces weight gain/loss and works together with our other body’s cells. As the science grows here we will have a much greater understanding of our body’s weight loss mechanisms. Once we do that, then we can better help people with this disease.
Diet and Exercise: Don’t Do It? Part II
2300 words
In part II, we will look at the mental gymnastics of someone who is clueless to the data and uses whatever mental gymnastics possible in order to deny the data. Well, shit doesn’t work like that, JayMan. I will review yet more studies on sitting, walking and dieting on mortality as well as behavioral therapy (BT) in regards to obesity. JayMan has removed two of my comments so I assume the discussion is over. Good thing I have a blog so I can respond here; censorship is never cool. JayMan pushes very dangerous things and they need to be nipped in the bud before someone takes this ‘advice’ who could really benefit from lifestyle alterations. Stop giving nutrition advice without credentials! It’s that simple.
JayMan published a new article on ‘The Five Laws of Behavioral Genetics‘ with this little blip:
Indeed, we see this with health and lifestyle: people who exercise more have fewer/later health problems and live longer, so naturally conventional wisdom interprets this to mean that exercise leads to health and longer life, when in reality healthy people are driven to exercise and have better health due to their genes.
So, in JayMan’s world diet and exercise have no substantial impact on health, quality of life and longevity? Too bad the data says otherwise. Take this example:
Take two twins. Lock both of them in a metabolic chamber. Monitor them over their lives and they do not leave the chamber. They are fed different diets (one has a high-carb diet full of processed foods, the other a healthy diet for whatever activity he does); one exercises vigorously/strength trains (not on the same day though!) while the other does nothing and the twin who exercises and eats well doesn’t sit as often as the twin who eats a garbage diet and doesn’t exercise. What will happen?
Jayman then shows me Bouchard et al, (1990) in which a dozen pairs of twins were overfed for three months with each set of twins showing different gains in weight despite being fed the same amount of kcal. He also links to Bouchard et al, 1996 (can’t find the paper; the link on his site is dead) which shows that the twins returned to their pre-experiment weight almost effortlessly. This, of course, I do not deny.
This actually replicates a study done on prisoners in a Vermont prison (Salans, Horton, and Sims, 1971). “The astonishing overeating paradox” is something that’s well worth a look in to. Salans et al had prisoners overeat and also limited their physical activity. They started eating 4000 kcal per day and by the end of the study they were eating about 10000 kcal per day. But something weird happened: their metabolisms revved up by 50 percent in an attempt to get rid of the excess weight. After the study, the prisoners effortlessly returned to their pre-experiment weight—just like the twins in Bouchard et al’s studies.
The finding is nothing new but it’s nice to have replication (on top of the replication that it already had), but that’s not what I was talking about. Of course, being sedentary, eating like shit and not exercising will lead to deleterious health outcomes. The fact of the matter is, the twin in my thought experiment that did not exercise, sat around all day and ate whatever would die way sooner, have a lower quality of life, and more deleterious disease due to the shitty diet while his co-twin would have less since he ate right, exercised and spent less time sitting.
JayMan says, in regards to studies that show that obese people that even do light physical activity show lower all-cause mortality, that “That’s not what large RCTs show.” I know the study that he’s speaking of—the Look AHEAD study (Action for Health and Diabetes) (The Look AHEAD Research Group, 2009). The research group studied the effects of lifestyle interventions in type II diabetics. For one of the groups they gave intensive diet and exercise information, the other they gave only the standard advice. However, the study ended early at 9.3 years because there was no difference between both groups (Pi-Sunyer, 2015). JayMan uses this study as evidence that diet and exercise have no effect on the mortality of type II diabetics; however, in actuality, the results are much more nuanced.
Annuzzi et al (2014) write in their article The results of Look AHEAD do not row against the implementation of lifestyle changes in patients with type 2 diabetes:
The intervention aimed at weight loss by reducing fat calories, and using meal replacements and, eventually, orlistat, likely underemphasizing dietary composition. There is suggestive evidence, in fact, that qualitative changes in dietary composition aiming at higher consumption of foods rich in fiber and with a high vegetable/animal fat ratio favorably influence CV risk in T2D patients.
In conclusion, the Look AHEAD showed substantial health benefits of lifestyle modifications. Prevention of CV events may need higher attention to dietary composition, contributing to stricter control of CV risk factors. As a better health-related quality of life in people with diabetes is an important driver of our clinical decisions, efforts on early implementation of behavioral changes through a multifactorial approach are strongly justified.
They reduced far calories and used meal replacements. This is the trial JayMan is hedging his assertion on. Type II diabetics need a higher fat diet and don’t need the carbs as it will spike their insulin. Eating a higher fat diet will also lower the rate of CVD as well. This trial wasn’t too vigorous in terms of macronutrient composition. This is one of many reasons why type II diabetics discard dieting and exercise just yet.
Even modest weight loss of 5 to 10 percent is associated with significant improvements in cardiovascular disease (CVD) after one year, with larger weight loss showing better improvement (Wing et al, 2011). (Also read the article The Spinning of Look AHEAD.)
Telling diabetics not to eat right and exercise is, clearly, a recipe for disaster. This canard that dieting/exercise doesn’t work to decrease all-cause mortality—especially for diabetics and others who need the lifestyle interventions—is dangerous and a recipe for disaster.
Intentional weight loss needs to be separated from intentional weight loss as to better study the effects of both variables. Kritchevsky et al (2015) meta-analyzed 15 RCTs that “reported mortality data either as an endpoint or as an adverse event, including study designs where participants were randomized to weight loss or non-weight loss, or weight loss plus a co-intervention (e.g. weight loss plus exercise) or the weight stable co-intervention (i.e. exercise alone).” They conclude that the risk for all-cause mortality in obese people who intentionally lose weight is 15 percent lower than people not assigned to lose weight.
This study replicates a meta-analysis by Harrington, Gibson, and Cottrell (2009) on the benefits of weight loss and all-cause mortality. They noted that in unhealthy adults, weight loss accounted for a 13 percent decrease in all-cause mortality increase while in the obese this accounted for a 16 percent decrease. Of course, since the weights were self-reported and there are problems with self-reports of weight (Mann et al, 2007), then that is something that a skeptic can rightfully bring up. However, it would not be a problem since this would imply that they weighed the same/gained more weight yet had a decrease in all-cause mortality.
Even light physical activity is associated with a decrease in all-cause mortality. People who go from light activity, 2.5 hours a week of moderate physical intensity compared to no activity, show a 19 percent decrease in all-cause mortality while people who did 7 hours a week of moderate activity showed a 24 percent decrease in all-cause mortality (Woodcock et al, 2011). Even something as simple as walking is associated with lower incidence of all-cause mortality, with the largest effect being seen in individuals who went from no activity to light walking. Walking is inversely associated with disease incidence (Harner and Chida, 2008) but their analysis indicated publication bias so further study is needed. Nevertheless, the results line up with what is already known—that low-to-moderate exercise is associated with lower all-cause mortality (as seen in Woodcock et al, 2011).
What is needed to change habits/behavior is behavioral therapy (BT) (Jacob and Isaac, 2012; Buttren, Webb, and Waddren, 2012; Wilfley, Kolko, and Kaas, 2012; ). BT can also be used to increase adherence to exercise (Grave et al, 2011). BT has been shown to have great outcomes in the behaviors of obese people, and even if no weight loss/5-10 percent weight loss is seen (from Wing and Hill, 2001), better habits can be developed, and along with ‘training’ hunger hormones with lifestyle changes such as fasting, people can achieve better health and longevity—despite what naysayers may say. Though I am aware that outside of clinics/facilities, BT does not have a good track record (Foster, Makris, and Bailer, 2005). However, BT is the most studied and effective intervention in managing obesity at present (Levy et al, 2007). This is why people need to join gyms and exercise around people—they will get encouragement and can talk to others about their difficulties. Though, people like JayMan who have no personal experience doing this would not understand this.
In regards to dieting, the effect of macronutrient composition on blood markers is well known. Type II diabetics need to eat a certain diet to manage their insulin/blood sugar, and doing the opposite of those recommendations will lead to disaster.
Low-carb ketogenic diets are best for type II diabetics. There are benefits to having ketones circulating in the blood, which include (but are not limited to): weight loss, improved HbA1c levels, reduced rate of kidney disease/damage, cardiac benefits, reversing non-alcoholic fatty liver, elevated insulin, and abnormal levels of cholesterol in the blood (Westman et al, 2008; Azar, Beydoun, and Albadri, 2016; Noakes and Windt, 2016; Saslow et al, 2017). These benefits, of course, carry over to the general non-diabetic population as well.
Of course, JayMan has reservations about these studies wanting to see follow-ups—but the fact of the matter is this: dieting and eating right is associated with good blood markers, exactly what type II diabetics want. In regards to food cravings, read this relevant article by Dr. Jason Fung: Food Cravings. Contrary to JayMan’s beliefs, it’s 100 percent possible to manage food cravings and hunger. The hormone ghrelin mediates hunger. There are variations in ghrelin every day (Natalucci et al, 2005) and so if you’re feeling hungry if you wait a bit it will pass. This study lines up with most people’s personal experience in regards to hunger. One would have to have an understanding of how the brain regulates appetite to know this, though.
JayMan also cannot answer simple yes or no questions such as: Are you saying that people should not watch what they eat and should not make an effort to eat higher-quality foods? I don’t know why he is so anti-physical activity. As if it’s so bad to get up, stop sitting so much and do some exercise! People with more muscle mass and higher strength levels live longer (Ruiz et al, 2008). This anti-physical activity crusade makes absolutely no sense at all given the data. If I were to stop eating well and strength training, along with becoming a couch potato, would my chance of dying early from a slew of maladies decrease? Anyone who uses basic logic would be able to infer that the answer is yes.
I also need to address JayMan’s last comment to me which he censored:
No intervention shows that lifestyle changes extend life – or even improve health. Even if they did, their generalizability would depend on their actual prescription. In any case, the point is moot, since they don’t even show such improvements in the first place.
You’re only saying that because you’re literally hand waving away data. It’s clear that going from no exercise to some exercise will decrease all-cause mortality. I’m sorry that you have a problem reading and understanding things that you don’t agree with, but this is reality. You don’t get to construct your own reality using cherry-picked studies that don’t mean what you think they mean (like Look AHEAD; Dr. Sharma states that we may never know if weight reduction can save lives in type II diabetics, however the three studies on low-carb diets cited above lend credence to the idea that we can).
Please see my previously linked Obesity Facts page for more. Once you’ve read that, get back to me. Until then, I’m putting the brakes on this discussion.
Of course, you’re putting the brakes on this discussion, you have substantial replies other than your one-liners. You need to censor people when you have no substantial response, that’s not intellectually honest.
All in all, JayMan is giving very dangerous ‘advice’, when the literature says otherwise in regards to lifestyle interventions and all-cause mortality. You can talk about genes for this or that all you want; you’re just appealing to genes. Light physical exercise shows that mortality risk can be decreased; that’s not too hard for most people.
I know JayMan talks about genes for this and that, yet he does not understand that obesogenic environments drive this epidemic (Lake and Townshend, 2006; Powell, Spears, and Rebori, 2011; Fisberg et al, 2016). He doesn’t seem to know about the food reward hypothesis of obesity either. Think about obesogenic environments and food reward and how our brains change when we eat sugar and then things will begin to become clearer.
JayMan is giving out deadly ‘advice’, again, without the correct credentials. Clearly, as seen in both of my responses to him, taking that ‘advice’ will lead to lower quality of life and lower life expectancy. But I’m sure my readers are smart enough to not listen to such ‘advice’.
(Note: Diet and exercise under Doctor’s supervision only)
The ENA Theory: On Testosterone and Aggressive Behavior by Race/Ethnicity
3250 words
A commenter by the name of bbloggz alerted me to a new paper by Lee Ellis published this year titled Race/ethnicity and criminal behavior: Neurohormonal influences in which Ellis (2017) proposed his theory of ENA (evolutionary neuroandrogenic theory) and applied it to racial/ethnic differences in crime. On the face, his theory is solid and it has great explanatory power for the differences in crime rates between men and women, however, there are numerous holes in the application of the theory in regards to racial/ethnic differences in crime.
In part I, he talks about racial differences in crime. No one denies that, so on to part II.
In part II he talks about environmental causes for the racial discrepancies, that include economic racial disparities, racism and societal discrimination and subordination, a subculture of violence (I’ve been entertaining the honor culture hypothesis for a few months; Mazur (2016) drives a hard argument showing that similarly aged blacks with some college had lower levels of testosterone than blacks with less than high school education which fits the hypothesis of honor culture. Though Ellis’ ENA theory may account for this, I will address this below). However, if the environment that increases testosterone is ameliorated (i.e., honor culture environments), then there should be a subsequent decrease in testosterone and crime, although I do believe that testosterone has an extremely weak association with crime, nowhere near high enough to account for racial differences in crime, the culture of honor could explain a good amount of the crime gap between blacks and whites.
Ellis also speaks about the general stress/strain explanation, stating that blacks have higher rates of self-esteem and Asians the lowest, with that mirroring their crime rates. This could be seen as yet another case for the culture of honor in that blacks with a high self-esteem would feel the need to protect their ‘name’ or whatever the case may be and feel the need for physical altercation based on their culture.
In part III, Ellis then describes his ENA theory, which I don’t disagree with on its face as it’s a great theory with good explanatory power but there are some pretty large holes that he rightly addresses. He states that, as I have argued in the past, females selected men for higher rates of testosterone and that high rates of testosterone masculinize the brain, changing it from its ‘default feminine state’ and that the more androgens the brain is exposed to, the more likely it is for that individual to commit crime.
Strength
Ellis cites a study by Goodpaster et al (2006) in which he measured the races on the isokinetic dynamometry, pretty much a leg extension. However, one huge confound is that participants who did not return for follow-up were more likely to be black, obese and had more chronic disease (something that I have noted before in an article on racial grip strength). I really hate these study designs, but alas, it’s the best we have to go off of and there are a lot of holes in them that must be addressed. Though I applaud the researchers’ use of the DXA scan (regular readers may recall my criticisms on using calipers to assess body fat in the bench press study, which was highly flawed itself; Boyce et al, 2014) to assess body fat as it is the gold standard in the field.
Ellis (2017: 40) writes: “as brain exposure to testosterone surges at puberty, the prenatally-programmed motivation to strive for resources, status, and mating opportunities will begin to fully activate.” This is true on the face, however as I have noted the correlation between physical aggression and testosterone although positive is low at .14 (Archer, 1991; Book et al, 2001). Testosterone, as I have extensively documented, does cause social dominance and confidence which do not lead to aggression. However, when other factors are coupled with high testosterone (as noted by Mazur, 2016), high rates of crime may occur and this may explain why blacks commit crime; a mix of low IQ, high testosterone and low educational achievement making a life of crime ‘the smart way’ to live seeing as, as Ellis points out, and that intelligent individuals find legal ways to get resources while less intelligent individuals use illegal ways.
ENA theory may explain racial differences in crime
In part IV he attempts to show how his ENA theory may explain racial differences in crime—with testosterone sitting at the top of his pyramid. However, there are numerous erroneous assumptions and he does rightly point out that more research needs to be done on most of these variables and does not draw any conclusions that are not warranted based on the data he does cite. He cites one study in which testosterone levels were measured in the amniotic fluid of the fetus. The sample was 59 percent white and due to this, the researchers lumped blacks, ‘Hispanics’ and Native Americans together which showed no significant difference in prenatal testosterone levels (Martel and Roberts, 2014).
Umbilical cord and testosterone exposure
Ellis then talks about testosterone in the umbilical cord, and if the babe is exposed to higher levels of testosterone in vitro, then this should account for racial/ethnic differences in crime. However, the study he cited (Argus-Collins et al, 2012) showed no difference in testosterone in the umbilical cord while Rohrmann et al (2009) found no difference in testosterone between blacks and whites but found higher rates of SHBG (sex hormone-binding globulin) which binds to testosterone and makes it unable to leave the blood which largely makes testosterone unable to affect organ development. Thusly, if the finding of higher levels of SHBG in black babes is true, then they would be exposed to less androgenic hormones such as testosterone which, again, goes against the ENA theory.
He also cites two more studies showing that Asian babes have higher levels of umbilical cord testosterone than whites (Chinese babes were tested) (Lagiou et al, 2011; Troisi et al, 2008). This, again, goes against his theory as he rightly noted.
Circulating testosterone
Next he talks about circulating differences in testosterone between blacks and whites. He rightly notes that testosterone must be assayed in the morning within an hour after waking as that’s when levels will be highest, yet cites Ross et al (1986) where assay times were all over the place and thusly testosterone cannot be said to be higher in blacks and whites based on that study and should be discarded when talking about racial differences in testosterone due to assay time being between 10 am and 3 pm. He also cites his study on testosterone differences (Eliss and Nyborg, 1993), but, however, just as Ross et al (1986) did not have a control for WC (waist circumference) Ellis and Nyborg (1993) did not either, so just like the other study that gets cited to show that there is a racial difference in testosterone, they are pretty hugely flawed and should not be used in discussion when discussing racial differences in testosterone. Why do I not see these types of critiques for Ross et al (1986) in major papers? It troubles me…
He also seems to complain that Lopez et al (2013) controlled for physical activity (which increases testosterone) and percent body fat (which, at high levels, decreases testosterone). These variables, as I have noted, need to be controlled for. Testosterone varies and fluctuated by age; WC and BMI vary and fluctuate by age. So how does it make sense to control for one variable that has hormone levels fluctuate by age and not another? Ellis also cites studies showing that older East Asian men had higher levels of testosterone (Wu et al, 1995). Nevertheless, there is no consensus; some studies show Chinese babes have higher levels of testosterone than whites and some studies show that whites babes have higher levels of testosterone than Chinese babes. Indeed, this meta-analysis by Ethnicmuse shows that Asians have the highest levels, followed by Africans then Europeans, so this needs to be explained to save the theory that testosterone is the cause of black overrepresentation of violence (as well as what I showed that testosterone is important for vital functioning and is not the boogeyman the media makes it out to be).
Bone density and crime
Nevertheless, the next variable Ellis talks about is bone density and its relationship to crime. Some studies find that blacks are taller than whites while other show no difference. Whites are also substantially taller than Asian males. Blacks have greater bone density than the other three races, but according to Ellis, this measure has not been shown to have a relationship to crime as of yet.
Penis size, race and crime
Now on to penis size. In two articles, I have shown that there is no evidence for the assertion that blacks have larger penises than whites. However, states that penis length was associated with higher levels of testosterone in Egyptian babes. He states that self-reported penis size correlates with self-reports of violent delinquency (Ellis and Das, 2012). Ellis’ main citations for the claim that blacks have larger penises than other races comes from Nobile (1982), the Kinsey report, and Rushton and Boagert (1987) (see here for a critique of Rushton and Boagert, 1987), though he does cite a study stating that blacks had a longer penis than whites (blacks averaging 5.77 inches while whites averaged 5.53 inches). An HBDer may go “Ahah! Evidence for Rushton’s theory!”, yet they should note that the difference is not statistically significant; just because there is a small difference in one study also doesn’t mean anything for the totality of evidence on penis size and race—that there is no statistical difference!
He then cites Lynn’s (2013) paper which was based on an Internet survey and thus, self-reports are over-measured. He also cites Templer’s (2002) book Is Size Important?, which, of course, is on my list of books to read. Nevertheless, the ‘evidence’ that blacks average larger penises than whites is extremely dubious, it’s pretty conclusive that the races don’t differ in penis size. For further reading, read The Pseudoscience of Race Differences in Penis Size, and read all of Ethnicmuses’ posts on penis size here. It’s conclusive that there is no statistical difference—if that—and any studies showing a difference are horribly flawed.
2d/4d ratio and race
Then he talks about 2d/4d ratio, which supposedly signifies higher levels of androgen exposure in vitro (Manning et al, 2008) however these results have been challenged and have not been replicated (Koehler, Simmons, and Rhodes, 2004; Yan et al, 2008, Medland et al, 2010). Even then, Ellis states that in a large analysis of 250,000 respondents, Asians had the lowest 2d/4d ratio, which if the hypothesis of in vitro hormones affecting digit length is to be believed, they have higher levels of testosterone than whites (the other samples had small ns, around 100).
Prostate-specific antigens, race, and prostate cancer
He then talks about PSA (prostate-specific antigen) rates between the races. Blacks are two times more likely to get prostate cancer, which has been blamed on testosterone. However, I’ve compiled good evidence that the difference comes down to the environment, i.e., diet. Even then, there is no evidence that testosterone causes prostate cancer as seen in two large meta-analyses (Stattin et al, 2003; Michaud, Billups, and Partin, 2015). Even then, rates of PCa (prostate cancer) are on the rise in East Asia (Kimura, 2012; Chen et al, 2015; Zhu et al, 2015) which is due to the introduction of our Western diet. I will cover the increases in PCa rates in East Asia in a future article.
CAG repeats
He then reviews the evidence of CAG repeats. There is, however, no evidence that the number of CAG repeats influences sensitivity to testosterone. However, intra-racially, lower amounts of CAG repeats are associated with higher spermatozoa counts—but blacks don’t have higher levels of spermatozoa (Mendiola et al, 2011; Redmon et al, 2013). Blacks do have shorter CAG repeats, and this is consistent with the racial crime gap of blacks > whites > Asians. However, looking at the whole of the evidence, there is no good reason to assume that this has an effect on racial crime rates.
Intelligence and education
Next he talks about racial differences in intelligence and education, which have been well-established. Blacks did have higher rates of learning disabilities than whites who had higher levels of learning disabilities then Asians in a few studies, but other studies show whites and South Asians having different rates, for instance. He then talks about brain size and criminality, stating that the head size of males convicted for violent crimes did not differ from males who committed non-violent crimes (Ikaheimo et al, 2007). I won’t bore anyone with talking about what we know already: that the races differ in average brain size. However, a link between brain size and criminality—to the best of my knowledge—has yet to been discovered. IQ is implicated in crime, so I do assume that brain size is as well (no matter if the correlation is .24 or not; Pietschnig et al, 2015).
Prenatal androgen exposure
Now to wrap things up, the races don’t differ in prenatal androgen exposure, which is critical to the ENA theory; there is a small difference in the umbilical cord favoring blacks, and apparently, that predicts a high rate of crime. However, as noted, blacks have higher levels of SHBG at birth which inhibits the production of testosterone on the organs. Differences in post-pubertal testosterone are small/nonexistent and one should not talk about them when talking about differences in crime or disease acquisition such as PCa. DHT only shows a weak positive correlation with aggression—the same as testosterone (Christiansen and Winkler, 1992; however other studies show that DHT is negatively correlated with measures of physical aggression; Christiansen and Krussmann, 1987; further, DHT is not so evil after all).
Summing it all up
Blacks are not stronger than whites, indeed evidence from the races’ differing somatype, grip strength and leverages all have to do with muscular strength. Furthermore, the study that Ellis cites as ‘proof’ that blacks are stronger than whites is on one measure; an isokinetic dynamometry machine which is pretty much a leg extension. In true tests of strength, whites blow blacks away, which is seen in all major professional competitions all around the world. Blacks do have denser bones which is due to androgen production in vitro, but as of yet, there has been no research done into bone density and criminality.
The races don’t differ on penis size—and if they do it’s by tenths of an inch which is not statisitcally significant and I won’t waste my time addressing it. It seems that most HBDers will see a racial difference of .01 and say “SEE! Rushton’s Rule!” even when it’s just that, a small non-significant difference in said variable. That’s something I’ve encountered a lot in the past and it’s, frankly, a waste of time to converse about things that are not statistically significant. I’ve also rebutted the theory on 2d/4d ration as well. Finally, Asians had a similar level of androgen levels compared to blacks, with whites having the least amount. Along with a hole in the theory for racial differences in androgen causing crime, it’s yet another hole in the theory for racial differences in androgens causing racial differences in penis size and prostate cancer.
On intelligence scores, no one denies that blacks have scored about 1 SD lower than whites for 100 years, no one denies that blacks have a lower educational attainment. In regards to learning disabilities, blacks seem to have the highest rates, followed by Native Americans, than non-Hispanic whites, East Asians and the lowest rates found in South Asians. He states only one study links brain size to criminal behavior and it showed a significant inverse relationship with crime but not other types of offenses.
This is a really good article and I like the theory, but it’s full of huge holes. Most of the variables described by Ellis have been shown to not vary at all or much between the races (re: penis size, testosterone, strength [whites are stronger] prostate cancer caused mainly by diet, 2d/4d ratio [no evidence of it showing a digit ratio difference], and bone density not being studied). Nevertheless, a few of his statements do await testing so I await future studies on the matter. He says that androgen exposure ‘differs by race and ethnicity’, yet the totality of evidence shows ‘not really’ so that cannot be the cause of higher amounts of crime. Ellis talks about a lot of correlates with testosterone, but they do not pass the smell test. Most of it has been rebutted. In fact, one of the central tenets of the ENA theory is that the races should differ in 2d/4d ratio due to exposure of differing levels of the hormone in vitro. Alas, the evidence to date has not shown this—it has in fact shown the opposite.
ENA theory is good in thought, but it really leaves a lot to be desired in regards to explaining racial differences in crime. More research needs to be looked into in regards to intelligence and education and its effect on crime. We can say that low IQ people are more likely to drop out of school and that is why education is related to crime. However, in Mazur (2016) shows that blacks matched for age had lower levels of testosterone if they had some college under their belt. This seems to point in the direction of the ENA theory, however then all of the above problems with the theory still need to be explained away—and they can’t! Furthermore, one of the nails in the coffin should be this: East Asian males are found to have higher levels of testosterone than white males, often enough, and East Asian males actually have the lowest rate of crime in the worle!
This seems to point in the direction of the ENA theory, however then all of the above problems with the theory still need to be explained away—and they can’t! Furthermore, one of the nails in the coffin should be this: East Asian males are found to have higher levels of testosterone than white males, often enough, and East Asian males actually have some of the lowest rate of crime in the world (Rushton, 1995)! So this is something that needs to be explained if it is to be shown that testosterone facilitates aggression and therefore, crime.
Conclusion
I’ve shown—extensively—that there is a low positive correlation between testosterone and physical aggression, why testosterone does not cause crime, and have definitively shown that, by showing how flawed the other studies are that purport to show blacks have higher testosterone levels than whites, along with citing large-scale meta-analyses, that whites and blacks either do not differ or the differences is small to explain any so-called differences in disease acquisition or crime. One final statement on the CAG repeats, they are effect by obesity, men who had shorter CAG repeats were more likely to be overweight, which would skew readings (Gustafsen, Wen, and Koppanati, 2003). So depending on the study—and in most of the studies I cite whites have a higher BMI than blacks—BMI and WC should be controlled for due to the depression of testosterone.
It’s pretty conclusive that testosterone itself does not cause crime. Most of the examples cited by Ellis have been definitively refuted, and his other claims lack evidence at the moment. Even then, his theory rests on the 2d/4d ratio and how blacks may have a lower 2d/4d ratio than whites. However, I’ve shown that there is no significant relationship between 2d/4d ratio and traits mediated by testosterone (Kohler, Simmons, and Rhodes, 2004) so that should be enough to put the theory to bed for good.
Rebutting Heartiste on the Twinkie Diet
1300 words
Nutritional myths run amok everywhere. One of the most persistent is that ‘a calorie is a calorie’, that is, every macronutrient will be processed the same by the body. Another assumption is that the body doesn’t ‘care’ about where the calories come from—they can come from fat, protein, or carbs and the response will be the same: bodyweight will be reduced until one reaches their goal. However, it’s not as simple as that. He also has the assumption that “diets work”, when the best meta-analysis I know of on the matter shows the opposite (Mann et al, 2007, see especially table 1). They control for studies where weight was self-reported. They conclude that dieting does not work. This is what, as Heartiste says, “iScience!” says on the matter, so he should believe everything I state in this article, which is backed by “iScience!”.
Chateau Heartiste published an article back in 2010 titled The Twinkies Diet Proves Fatty Fats Are Fat Because They Eat Too Much. He is referring to professor of human nutrition Mark Haub and his success on ‘the twinkies diet’, where 2/3rds of his caloric intake came from junk food such as Twinkies. He lost 27 pounds in a two month period while his LDL cholesterol decreased by 20 percent and his HDL cholesterol increased by 20 percent. His level of triglycerides also decreased by 37 percent, with his body fat decreasing from 33.4 to 24.9 percent. So he ate 1800 kcal per day—2/3rds of it being junk food—for two months and lost 27 pounds. Case closed, right? Eat junk food at a deficit and lose weight? A calorie is a calorie? There are a few problems with this contention which will be addressed below.
Heartiste writes:
Big bottom line: Being fat itself is bad for your health. “Fat and fit” is a myth. The change that counts the most is losing the weight, which can only be done by PUSHING AWAY FROM THE TABLE.
Except fit and overweight and obese individuals have similar mortality rates than their normal weight counterparts (Barry et al, 2014). However, more recently a study was published purporting that overweight and obese individuals being healthy despite excess weight is a myth. The researchers state that in a sample of millions of Britons that overweight and obese individuals had a higher risk of heart disease than their normal-weight counterparts. Unfortunately, I cannot locate the study since it wasn’t published in a journal (and thusly not peer reviewed). I wonder if variables such as diet, smoking and other lifestyle factors were taken into account. Nevertheless, the debate on fitness and fatness continues.
Another large meta-analysis shows that grade 1 obesity (BMI 30->35) had the same mortality risk as normal-weight individuals with grade 2 obese (BMI +35) having a significantly higher risk of death (Flegal, Kit, and Orpana, 2013).
Heartiste claims that ‘a calorie is a calorie’. This is a common fallacy. This suggests that the body will process all foods the same way—that is, processing them the same metabolically. This, however, is not the case. Haub himself is a sample size of 1. If Heartiste can use a sample size of 1 to make a claim, then I can too.
Sam Feltham ate +5,000 kcal per day for 21 days and only gained 1.3 kg when he should have gained 7.3 kg based on the amount of kcal he ate. A calorie is a calorie, right? This is a fallacious statement. The statement “a calorie is a calorie” violates the second law of thermodynamics (Feinman and Fine, 2004). Heartiste writes:
That first law of thermodynamics looms large over everything.
The first law of thermodynamics is irrelevant to human physiology. It only states that an organism gets bigger if it consumes more energy; it doesn’t state why this occurs, which is due to the hormone insulin which causes weight gain.
He does rightly state that an omega 3/6 imbalance is part of the reason but then handwaves it away. Western-like high-fat diets (i.e., diets with an imbalance of linoleic acids (LA; and n-6 fatty acid) with n-3) are sufficient enough to induce gradual enhancement in fat mass across the generations (Massiera et al, 2010). This obviously includes the average 55 percent carbohydrate diet that the AHA recommends (Eckel et al, 2014). The Standard American Diet (aptly named the “SAD diet”) has the n-3/n-6 imbalance along with being high in carbohydrates which spike insulin which impedes fat being unlocked from the adipocyte.
Heartiste doesn’t understand that if you reduce the ‘in’, the ‘out’ also decreases. This was noted in the famous starvation experiment headed by Ancel Keys. They took 36 healthy men who ate normally for three months while being their behavior and personality was monitored. In the next six months, they were reduced to eating half of their initial intake (they started at 2000 kcal and dropped to 1000 kcal; some individuals going lower than that) and their metabolic rate decreased by 40 percent (Keys et al, 1945). This is proof for the contention that the body decreases its metabolic rate due to what is ingested. A similar study was done on Vermont prisoners, except they were told to gorge on food. Since they were in a controlled setting, the prisoners could be monitored to ensure they ate all of the food.
At the end of the study, their metabolic rates had increased by 50 percent. This is evidence that the body was trying to get back to its original weight. In six months, the prisoners went back to their normal weight as they ate normally (Salas, Horton, and Sims, 1971) One man only gained ten pounds eating all of those calories. Clearly, the body was resisting weight gain and when they were allowed to eat normally, they effortlessly regained their normal weights.
Finally, on the topic of Haub, Big Food shill, I will address a few things about him and his ‘research’ that recently came to light.
Intermittent fasting and obesity expert Dr. Jason Fung showed that in 2016 after Coca-Cola released their funding reports after criticisms of transparency, Mark Haub was found to be one of the many researchers that were backed by Coca-Cola. This is an attempt to show that ‘a calorie is a calorie’ and that ‘all calories are created equal’. This has been rebutted above.
In 2016—six years after his ‘experiment—it was revealed that he was funded by Coca-Cola. No doubt in order to ‘prove’ that ‘a calorie is a calorie’ and have people continue to gorge on high carbohydrate/insulinogenic foods. However, the human body is a lot more complex than to just reduce it to simply calories in and calories out—which I have written about in depth.
People like Heartiste need to get an actual understanding of the literature and what Coca-Cola has been trying to do for years, which is to make eating junk food ‘OK’ because ‘it doesn’t cause obesity’. Children consume 45 percent more food when exposed to advertisements (Harris, Bargh, and Brownell, 2009). So to begin to curb obesity rates we don’t need to ‘eat junk food’, we need to not eat junk food and eat a diet more ancestral to us—that is, one lower in processed carbs and higher in animal fat and protein. Big Food shills like Haub need to be exposed for what they are—people who do ‘research’ for a quick buck, i.e., not furthering our understanding of a complex issue as he would like you to believe. Exercise also doesn’t induce weight loss. So the claims of ‘eat less and move more’ (eat less according to the 55 percent carbohydrate recommendations) is bound to fail.
If Heartiste can make a claim using one man as an example then so can I. Read the above article by Sam Feltham in which he writes about hs experience eating 5,000 kcal per day for 21 days while only gaining 1.3 kg. I can use this example to say that eating low carb and high fat at 5,000 kcal per day will lead to negligible weight gain, however, I don’t use n=1 sample sizes to make claims and no one else should either.